Marco
Member
Hi cldlhd, Thanks for your post! I am 40 and have just found out hat I have severe aortic regurgitation which has led to decreased EF and a severely enlarged LV will need to have OHS soon. It came as a shock as I am extremely energetic, active and have never felt any fatigue symptoms. The cause is the aortic valve but it still remains unknown whether I have a BAV and additionally, whether my aortic root (3.9) will also need to be dealt with. I have just undergone further tests this week and will meet with the cardiologist again soon to know what they recommend. I have done research however and spoken to a few experts and these are my considerations:
1) Repair - if this is something both the cardiologist and surgeon say they can repair easily and have experience in doing then there's no doubt that this will be the best option, for all the reasons you have mentioned above and more. Even if they say that this will not be lifetime solution and that reoperation will be necessary in say 10-15 years, I will certainly still go for this option.
2) A Tissue valve - THese valves now last from 15-25 years and have the advantage over mechanical valves of not requiring long-time medication with Warfarin. This is my second best option - again it would mean reoperation when I am around 60 but I think (am still thinking about it, not sure) that to me that is preferable than the need for Warfarin and risks of infection, bleeding and complications if I need any other unrelated surgery or medication in the coming 15-20 years.
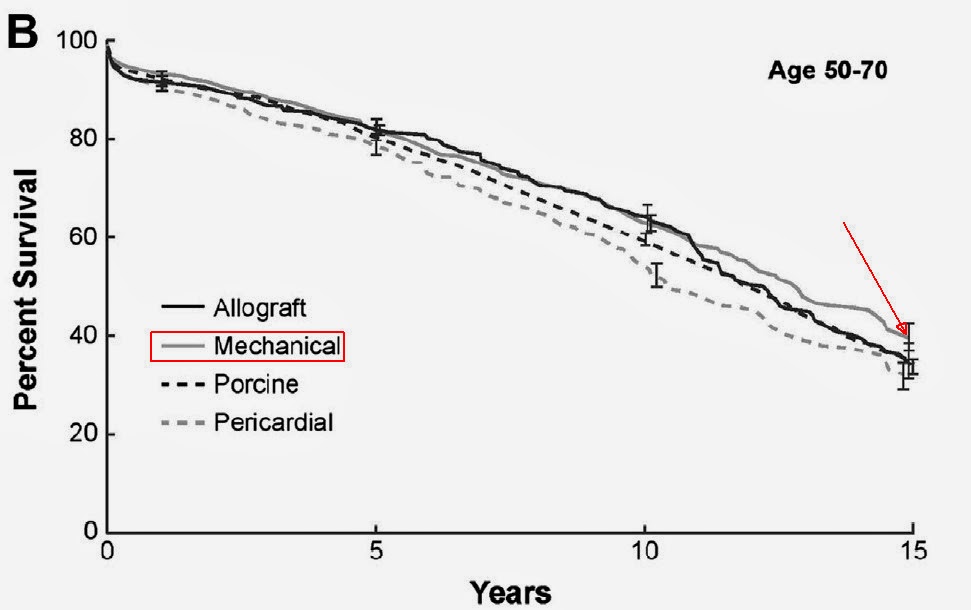
3) A mechanical valve - certainly has the advantage of being a lifelong solution, but there seems to be no evidence that the total lifespan is any different from people that have done repair or have tissue valves. Has the disadvantage of possible complications related to infections and Warfarin for the rest of your life, which of course many people find more than okay to live with.
So it really remains a personal -and no easy - choice! I will let you know what my surgeon suggests- -I will meet with him around the date you will meet with yours.
What option currently has your personal preference?
1) Repair - if this is something both the cardiologist and surgeon say they can repair easily and have experience in doing then there's no doubt that this will be the best option, for all the reasons you have mentioned above and more. Even if they say that this will not be lifetime solution and that reoperation will be necessary in say 10-15 years, I will certainly still go for this option.
2) A Tissue valve - THese valves now last from 15-25 years and have the advantage over mechanical valves of not requiring long-time medication with Warfarin. This is my second best option - again it would mean reoperation when I am around 60 but I think (am still thinking about it, not sure) that to me that is preferable than the need for Warfarin and risks of infection, bleeding and complications if I need any other unrelated surgery or medication in the coming 15-20 years.
3) A mechanical valve - certainly has the advantage of being a lifelong solution, but there seems to be no evidence that the total lifespan is any different from people that have done repair or have tissue valves. Has the disadvantage of possible complications related to infections and Warfarin for the rest of your life, which of course many people find more than okay to live with.
So it really remains a personal -and no easy - choice! I will let you know what my surgeon suggests- -I will meet with him around the date you will meet with yours.
What option currently has your personal preference?