MRiordan29
Member
Hi All,
This post is somewhat of a combination between valve selection, waiting room, and new advancements. I could write quite a bit here but I am going to try to give you the short version (I use that term loosely) for now.
I am 37 y/o and had my first OHS at 24 y/o to replace a bicuspid aortic valve which was first diagnosed as a child. I chose a tissue valve and had a Carpenter-Edwards Perimount 2800 implanted in June of 2006 at New York Presbyterian Weill-Cornell hospital in NYC. After an echo in April of this year, I learned that my tissue valve is severely stenotic and needs to be replaced. I went back to Weill-Cornell in May and met with a surgeon to discuss a re-op. I'm mostly asymptomatic but his recommendation was that I have it replaced before the end of the summer. My surgery is actually scheduled for Wednesday of this week, but I still have not made a valve selection and am also considering another option.
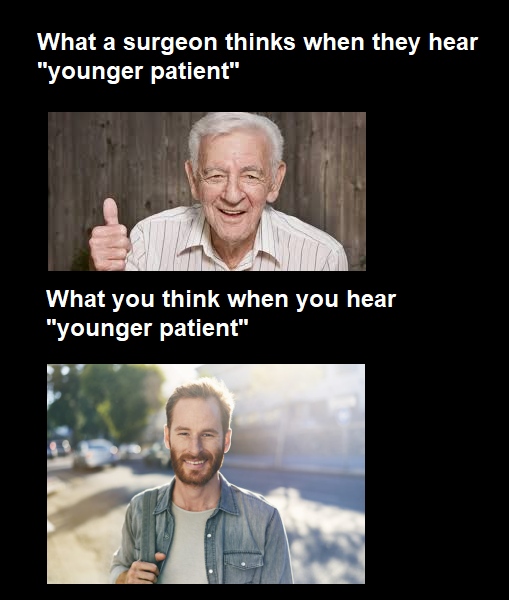
I have pretty much decided that I do not want to endure another OHS to get another tissue valve that will only last another 10 or 20 years, at which time I would be facing a third OHS. My initial inclination was to get a mechanical valve and hopefully be done with this. However, at the suggestion of my cardio I met with an Interventional Cardiologist that specializes in TAVR (aka TAVI). I was not expecting to be eligible for TAVR based on my age, low risk profile, and my knowledge of the general state of the technology. In fact, initially I was told that I am not eligible because the procedure has not been FDA approved for low-risk patients. Subsequently though, the doctor reached out to let me know that I could undergo TAVR as part of a registry within the current Carpenter-Edwards Sapien 3 Partner trial (I would not be part of the randomized trial) which is testing expansion of TAVR into low-risk patients. I was also told that I would need to submit to several tests (CAT scan, cardiac cath, etc.) to make sure that I am physically able to have TAVR. As mentioned above, I scheduled the traditional OHS but decided to proceed with the TAVR evaluation in the meantime since I would need most of the tests for the surgery regardless.
Subsequently, I met with the surgeon that oversees the TAVR program at Weill-Cornell. Basically they are presenting TAVR as having the same amount of risk as OHS but identified two main issues that they would be concerned about. First, that the valve doesn't end up in the correct position once inserted. The technology is such that they apparently are able to place the TAVR valves in the desired position almost every time, but it is not perfect and sometimes the valve ends up missing the desired landing site. Second, that the pressure gradient across the TAVR valve is too high once it is in place. This could happen because even though the TAVR valve has a very low profile, it would be inserted valve-in-valve into my current prosthetic valve which is 23 mm (so not small but also not large). The decreased opening could cause an increase in pressure across the new valve thus meaning I would have a stenotic TAVR valve right after it's put into place. Either of these problems would ultimately have to be corrected through OHS to take it all out and put in a new valve.
I had the cardiac cath, CAT scan, and ultrasound of my carotids. All of these came back normal and so I was expecting to get the approval for TAVR. However, in order to be part of the registry/trial, my tests had to be reviewed by a panel of doctors from around the country that are part of the trial. The panel asked for one additional test, a transesophageal echocardiogram (TEE) to make sure that there are no leaks around the ring of my current bio-prosthesis as that would make TAVR a bad idea. They don't have any specific reason to believe that I have such a leak but have asked for the test as a precaution. One logistical issue with this is that I can't have the TEE until 7/17, so I would have to delay my surgery in order to undergo the TEE and get a final answer as to my eligibility for TAVR.
Aside from the desire to avoid a second OHS, albeit temporarily, my main reason for even considering TAVR is to keep my options open going forward. Although there is no data to say how long the new generation of TAVR valves will last, especially in a young person, the thought is that they will last as long as the current traditional bio-prosthetic valves because the leaflets are made from the same tissue with the same treatments. Hypothetically, if this TAVR valve lasts me 10-15 years I would then be facing another choice. I could potentially have another valve-in-valve TAVR if there was enough space for that to happen, or a second OHS in which they would remove both valves and insert a new valve of my choice. My hope is that there would be an even better option available at that time, perhaps a second OHS but with a valve that will last the rest of my life and not require any anti-coagulation beyond an aspirin.
At the end of the day the TAVR comes with a lot of unknown and so I am not sure that I want to expose myself to that. I have read many of the relevant threads on this site as well as done some of my own research, and I just do not know how I feel about it. In terms of the OHS, it is relatively safe and a known entity. However, despite everything I have read on here and elsewhere I am still somewhat fearful of Coumadin, as irrational as that may sound. I have been looking into the On-X valve and am wondering if anyone has any input on that and the possibility of a reduction in the amount of anti-coagulation needed.
Anyhow, I would love to hear from anyone with thoughts, opinions, information, etc. I won't take offense if you think that I am crazy for even considering TAVR or for being in this position in the first place through my initial valve choice. I know that this is a respectful space and that no one here would say anything offensive, but time is short so I don't mind if you refrain from sugar-coating your thoughts. Thanks in advance for your help.
This post is somewhat of a combination between valve selection, waiting room, and new advancements. I could write quite a bit here but I am going to try to give you the short version (I use that term loosely) for now.
I am 37 y/o and had my first OHS at 24 y/o to replace a bicuspid aortic valve which was first diagnosed as a child. I chose a tissue valve and had a Carpenter-Edwards Perimount 2800 implanted in June of 2006 at New York Presbyterian Weill-Cornell hospital in NYC. After an echo in April of this year, I learned that my tissue valve is severely stenotic and needs to be replaced. I went back to Weill-Cornell in May and met with a surgeon to discuss a re-op. I'm mostly asymptomatic but his recommendation was that I have it replaced before the end of the summer. My surgery is actually scheduled for Wednesday of this week, but I still have not made a valve selection and am also considering another option.
I have pretty much decided that I do not want to endure another OHS to get another tissue valve that will only last another 10 or 20 years, at which time I would be facing a third OHS. My initial inclination was to get a mechanical valve and hopefully be done with this. However, at the suggestion of my cardio I met with an Interventional Cardiologist that specializes in TAVR (aka TAVI). I was not expecting to be eligible for TAVR based on my age, low risk profile, and my knowledge of the general state of the technology. In fact, initially I was told that I am not eligible because the procedure has not been FDA approved for low-risk patients. Subsequently though, the doctor reached out to let me know that I could undergo TAVR as part of a registry within the current Carpenter-Edwards Sapien 3 Partner trial (I would not be part of the randomized trial) which is testing expansion of TAVR into low-risk patients. I was also told that I would need to submit to several tests (CAT scan, cardiac cath, etc.) to make sure that I am physically able to have TAVR. As mentioned above, I scheduled the traditional OHS but decided to proceed with the TAVR evaluation in the meantime since I would need most of the tests for the surgery regardless.
Subsequently, I met with the surgeon that oversees the TAVR program at Weill-Cornell. Basically they are presenting TAVR as having the same amount of risk as OHS but identified two main issues that they would be concerned about. First, that the valve doesn't end up in the correct position once inserted. The technology is such that they apparently are able to place the TAVR valves in the desired position almost every time, but it is not perfect and sometimes the valve ends up missing the desired landing site. Second, that the pressure gradient across the TAVR valve is too high once it is in place. This could happen because even though the TAVR valve has a very low profile, it would be inserted valve-in-valve into my current prosthetic valve which is 23 mm (so not small but also not large). The decreased opening could cause an increase in pressure across the new valve thus meaning I would have a stenotic TAVR valve right after it's put into place. Either of these problems would ultimately have to be corrected through OHS to take it all out and put in a new valve.
I had the cardiac cath, CAT scan, and ultrasound of my carotids. All of these came back normal and so I was expecting to get the approval for TAVR. However, in order to be part of the registry/trial, my tests had to be reviewed by a panel of doctors from around the country that are part of the trial. The panel asked for one additional test, a transesophageal echocardiogram (TEE) to make sure that there are no leaks around the ring of my current bio-prosthesis as that would make TAVR a bad idea. They don't have any specific reason to believe that I have such a leak but have asked for the test as a precaution. One logistical issue with this is that I can't have the TEE until 7/17, so I would have to delay my surgery in order to undergo the TEE and get a final answer as to my eligibility for TAVR.
Aside from the desire to avoid a second OHS, albeit temporarily, my main reason for even considering TAVR is to keep my options open going forward. Although there is no data to say how long the new generation of TAVR valves will last, especially in a young person, the thought is that they will last as long as the current traditional bio-prosthetic valves because the leaflets are made from the same tissue with the same treatments. Hypothetically, if this TAVR valve lasts me 10-15 years I would then be facing another choice. I could potentially have another valve-in-valve TAVR if there was enough space for that to happen, or a second OHS in which they would remove both valves and insert a new valve of my choice. My hope is that there would be an even better option available at that time, perhaps a second OHS but with a valve that will last the rest of my life and not require any anti-coagulation beyond an aspirin.
At the end of the day the TAVR comes with a lot of unknown and so I am not sure that I want to expose myself to that. I have read many of the relevant threads on this site as well as done some of my own research, and I just do not know how I feel about it. In terms of the OHS, it is relatively safe and a known entity. However, despite everything I have read on here and elsewhere I am still somewhat fearful of Coumadin, as irrational as that may sound. I have been looking into the On-X valve and am wondering if anyone has any input on that and the possibility of a reduction in the amount of anti-coagulation needed.
Anyhow, I would love to hear from anyone with thoughts, opinions, information, etc. I won't take offense if you think that I am crazy for even considering TAVR or for being in this position in the first place through my initial valve choice. I know that this is a respectful space and that no one here would say anything offensive, but time is short so I don't mind if you refrain from sugar-coating your thoughts. Thanks in advance for your help.