Hi
heartburst;n867340 said:
I've had my St Jude's valve since April 1st and I'm feeling great. My INR has gone down to 1.5 a couple times. I think it will take sometime for my body to adjust.
your body does not adjust ... you do not build immunity or tolerance. So if anyone at a clinic has put that idea into your head they are wrong.
1.5 a couple of times is
mismanagement plain and simple. Please contact me by PM if you wish and I'll do my best to steer you straight on this.
My warfarin dose is a single 2.5mg pill per day, on Wednesdays I take 2. The clinic slightly increases the dose if I dip to low by doubling a single days dose.
common but not the correct approach ...
My question is: how dangerous is that if at all? Can clots form when INR is low and break free sometime later when INR is in range and do damage?
Ok, the short answer is
"its probably OK, but avoid it"
The logner answer is: I wouldn't advise it often but on very rare occasions the evidence (specifically around management of operations for those on warfarin) suggests that you should be OK
Basically it works like this: there are two ways clots can cause you difficulty:
- they form and adhere to the valve surface,
- they form in the blood and continue to grow before they are munched up by the body
so we with mech valves (just like Atrial Fibrilation patients) can form blood clots freely in the blood. In our case they are triggered by (among other things) the closing and opening jets of pressure caused by the valve. To see this, get a tap running gently, stick your thumb over it to block it. As you just about get it blocked it squirts out at high velocity (compared to its trickle). That's a Jet
So, when your INR is lower than 2 the possibility of this occuring increases. We know from the GELIA study that people with valves like you have who's INR was down to 1.7 reported no additional problems. These are early studies and its unwise to just leap in and do that yourself until we know how more general this applies to the population (likely that it does) and how it relates to you specifically (unknown without testing).
So that suggests that dips below 1.7 to (say) 1.5 would be unlikely to cause harm from strokes in the short term (meaning 1 or two days). None the less I'd avoid it.
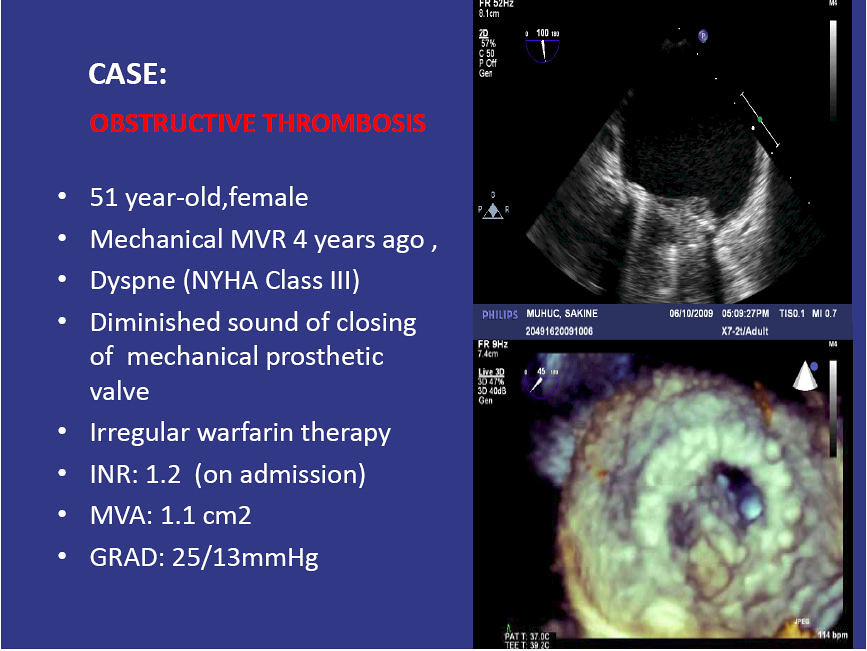
On the point of growth on the valve surface that's another issue which I don't believe that the GELIA study addresses. Thrombus is like snow, it attracts more thrombus. So if its ensconced on your valve it may grow. Below are two images of obstructive valve thrombosis:
This is obviously from a person with obstruction
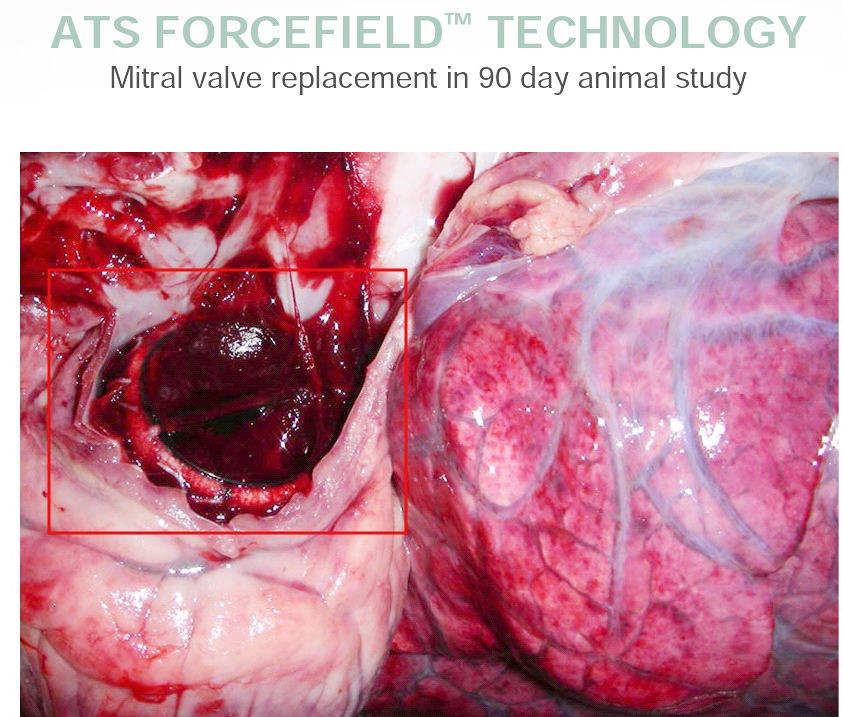
And then this is from an animal (if I recall correctly) which was used to demonstrate the accumulation of thrombus on the valve surface
you can see the surface of the valve is covered in a thin "paint" of thrombus, So to my understanding this accumulates with successive low INR events and is gradually washed off by blood flow when INR is higher (like over 2) in much the same manner as water flowing over rocks reduces the growths there..
So you
do not want to be at a low INR for lengthy periods (low meaning under 2 lengthy meaning days) for then this can build up and break off and then will be big enough to form a clot in blood vessel and cause you harm..