Superman
Well-known member
I've been on warfarin since I just turned 18. I'm 40 now and still have all of my hair.
Am I the only one that takes my dose in the morning? Always seemed to fit my routine better. I test weekly per the rules of my lab. I don't worry about diet, never really have. Hasn't changed lifestyle either, other than more freedom with a properly functioning valve. Was a pretty regular mountain biker in my 20's. Coach youth baseball, and have been drilled by the occasional line drive in coach pitch.
I'm in range pretty much every test. On the rare occasion that I'm out of range, I let the clinic think they've given me corrective advise, but then do what I think is right and get back in range.
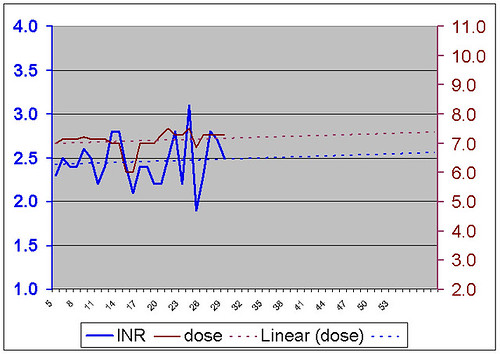
I think some of those that have a lot of trouble finding a proper dose are sometimes victims of mismanagement by their doctors as much as any unique metabolic circumstances. A bad warfarin manager can get the INR yo-yo started and can't find a way to stop it. They over correct, mess with your diet, and from one test to the next it's too high, then too low, etc.
It's okay to fire your manager. Find a different cardio, clinic, or turn it over to your primary care. Eventually people get comfortable enough with their own bodies response to dosing changes that the clinic really is just there for documentation purposes. Many long timers are self-managing.
Am I the only one that takes my dose in the morning? Always seemed to fit my routine better. I test weekly per the rules of my lab. I don't worry about diet, never really have. Hasn't changed lifestyle either, other than more freedom with a properly functioning valve. Was a pretty regular mountain biker in my 20's. Coach youth baseball, and have been drilled by the occasional line drive in coach pitch.
I'm in range pretty much every test. On the rare occasion that I'm out of range, I let the clinic think they've given me corrective advise, but then do what I think is right and get back in range.
I think some of those that have a lot of trouble finding a proper dose are sometimes victims of mismanagement by their doctors as much as any unique metabolic circumstances. A bad warfarin manager can get the INR yo-yo started and can't find a way to stop it. They over correct, mess with your diet, and from one test to the next it's too high, then too low, etc.
It's okay to fire your manager. Find a different cardio, clinic, or turn it over to your primary care. Eventually people get comfortable enough with their own bodies response to dosing changes that the clinic really is just there for documentation purposes. Many long timers are self-managing.