Double Post….
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Anyone in here in their mid 40's and what did your surgeon advise on valve type.
- Thread starter David W
- Start date

Help Support Valve Replacement Forums:
This site may earn a commission from merchant affiliate
links, including eBay, Amazon, and others.
Fundy
Well-known member
I'm far from an expert but I believe the tissue valves that are an actual pig valve, such as many of the mosaic's make the claim to be closest to human valve performance. Many heart centers still use and recommend these. I think it was the usual recommended tissue at Cleveland Clinic. I personally didn't want one of these types due to many 'installation' type of errors claimed and thus quicker redo times.
I have a St Jude Trifecta, I doubt its hemodynamic properties are causing me any problems.
Also on the warfarin necessary for a month or two after tissue valve. I thought this would be the case for me but found out that its not the recommendation for tissue in aortic position usually, but is usual for a tissue for mitral replacement. I've never had to take warfarin.
My main concern with the St Jude is that the company for some reason in the past applied some type of anti-clotting coating to one of their mechanical models which wasn't approved. And was subsequently determined to be cancer causing and recalled. At least one member posting here had one and was very unsatisfied with the companies response to the situation.
The surgeon's in my area have very good surgery history and to my knowledge go with St Jude valves most often. I was OK with the surgeon making the pick of which tissue valve to go with , providing that it wasn't of the type of the actual pig valves such as a Mosaic.
I'm guessing that those pig type of valves would be what you'd come up with as being the best in terms of blood flow mimicking the human valve, and there are many members here that have one of those that are quite happy with it. But again, the many early replacements usually blamed on the installation by the valve company scared me away from choosing them.
The St. Jude Trifecta uses both pig pericardium and cow pericardium tissue in its construction. The stent is first wrapped with pig, and then the actual valve material is formed from the cow tissue.
I have a St Jude Trifecta, I doubt its hemodynamic properties are causing me any problems.
Also on the warfarin necessary for a month or two after tissue valve. I thought this would be the case for me but found out that its not the recommendation for tissue in aortic position usually, but is usual for a tissue for mitral replacement. I've never had to take warfarin.
My main concern with the St Jude is that the company for some reason in the past applied some type of anti-clotting coating to one of their mechanical models which wasn't approved. And was subsequently determined to be cancer causing and recalled. At least one member posting here had one and was very unsatisfied with the companies response to the situation.
The surgeon's in my area have very good surgery history and to my knowledge go with St Jude valves most often. I was OK with the surgeon making the pick of which tissue valve to go with , providing that it wasn't of the type of the actual pig valves such as a Mosaic.
I'm guessing that those pig type of valves would be what you'd come up with as being the best in terms of blood flow mimicking the human valve, and there are many members here that have one of those that are quite happy with it. But again, the many early replacements usually blamed on the installation by the valve company scared me away from choosing them.
The St. Jude Trifecta uses both pig pericardium and cow pericardium tissue in its construction. The stent is first wrapped with pig, and then the actual valve material is formed from the cow tissue.
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
As an active 44 year old you stand the greatest chances of getting the minimum lifespan from any of the tissue prosthetics. Every evidence points towards earlier than manufacturer claimed calcification and stenosis with all of the tissue prosthetics.
http://mayo.img.entriq.net/htm/MayoPlayer1.html?articleID=4071
Note in particular his comments about active less than 50 years of age.
Make sure you are informing yourself to decide on merits, not feeding a decision already made
To my knowledge you seek The Grail. None exists and all are a compromise in one way or another.jumpy;n857957 said:As an active 44 year old as well, I am looking for something that mimics the flow of a natural valve.
As an active 44 year old you stand the greatest chances of getting the minimum lifespan from any of the tissue prosthetics. Every evidence points towards earlier than manufacturer claimed calcification and stenosis with all of the tissue prosthetics.
http://mayo.img.entriq.net/htm/MayoPlayer1.html?articleID=4071
Note in particular his comments about active less than 50 years of age.
Make sure you are informing yourself to decide on merits, not feeding a decision already made
Burto A.
New member
I'm 45 and I just had a mechanical valve installed. I figured I don't want to go through the entire process again in 15 or so years. And I may not have insurance that pays as well as mine does now.
I figured what's another pill to take every day. I was unaware of the complications that went with taking Coumadin (blood tests, watching what foods to eat/avoid). I'm still learning.
I was also unaware of the audible "ticking" of a mechanical valve. I am also still getting used to that. (If I am able to find a body position that eliminates the ticking I tend to stay like that as long as I can just for a piece-n-quiet timeout).
With everything that has changed in my life with a new valve I can still say I'm happy I went with the mechanical. I definitely wouldn't want to go through that surgery again, especially as and older man.
Good luck in your decision making and your up coming surgery.
I figured what's another pill to take every day. I was unaware of the complications that went with taking Coumadin (blood tests, watching what foods to eat/avoid). I'm still learning.
I was also unaware of the audible "ticking" of a mechanical valve. I am also still getting used to that. (If I am able to find a body position that eliminates the ticking I tend to stay like that as long as I can just for a piece-n-quiet timeout).
With everything that has changed in my life with a new valve I can still say I'm happy I went with the mechanical. I definitely wouldn't want to go through that surgery again, especially as and older man.
Good luck in your decision making and your up coming surgery.
I was in my early 30s and, fortunately for me, I didn't have a choice since only one mechanical valve was on the market and tissue valves where several years away. I didn't know then, and still don't know, the physics behind my valve function but the valve has never interfered with my occupation or lifestyle.....and I've pretty much completed my bucket list........on one surgery. I am not an exception as there are many mech. valves that have been in use for many decades. Warfarin is not difficult to manage and takes about 15 minutes a week.....that's less than a month over the 48 years I've had the valve. I wonder how many months I would have been in a hospital or recovery over those years with the several tissue valve re-ops I would have needed. That's a "loaded" question since a mechanical valve, almost certainly, would have been implanted after I had gone thru a couple tissue valves.
If you wish to minimize future surgeries consider a mechanical if you're young. If it doesn't matter to you and you don't want to take a pill a daily, choose tissue.
If you wish to minimize future surgeries consider a mechanical if you're young. If it doesn't matter to you and you don't want to take a pill a daily, choose tissue.
pellicle;n857961 said:Hi
To my knowledge you seek The Grail. None exists and all are a compromise in one way or another.
As an active 44 year old you stand the greatest chances of getting the minimum lifespan from any of the tissue prosthetics. Every evidence points towards earlier than manufacturer claimed calcification and stenosis with all of the tissue prosthetics.
http://mayo.img.entriq.net/htm/MayoPlayer1.html?articleID=4071
Note in particular his comments about active less than 50 years of age.
Make sure you are informing yourself to decide on merits, not feeding a decision already made
The only option that I can see that mimics the hemodynamics of the native valve unfortunately is the Ross. I started this thinking that it would be the better choice and then as a backup mechanical. Now I am opening up my research to all options as merits worthy of consideration. My own gut is telling me to avoid blood thinners but I'm certainly not thinking this over any one issue. The long term mortality rates are similar for Ross, mechanical and tissue. The re-operation rates that I can see are about 15% for the Ross and 9% for mechanical at 15 years. A broad statistical advantage to be sure but certainly nowhere in the region of tissue which would be closer to 50/50 at 15 years.
I meet with the surgeon in a couple of weeks so I want to go in without any decision made but I hope that my questions, his experience/history and my own gut feeling will help me to decide. At this point I feel further from deciding than ever….
pellicle
Professional Dingbat, Guru and Merkintologist
Hi Jumpy
actually, I agree with your premise - "unfortunately" ... The thing is that too will be a compromise as the tricuspid valve which is removed to replace the aortic valve does not have the same flow characteristics as the aorta, so if your hemodynamics is the key criteria (and please , I'd like to know why it is given so many athletes with mechanicals continue to do well in their sports) then it does not fit either.
Also, I'd be curious to know what you mean by hemodynamics, are you talking about opening / closing perssures, turbulence, closing velocity / opening velocity jets or are you just simply wanting it to carry as much blood?
What data do you have on the various valves and what do you see are the hemodynamic limitations of a modern bileaflet mechanical?
I can understand that, when I had my third valve put in I'd had a sense of dread about blood thinners instilled into me from surgeons in the preceding 20 years (NB from after my homograft). However when the third valve op surfaced suddenly that was brushed aside and "you'll need a mechanical" was all that was really left on the table logically.
I found this worrying, and have come to understand that the key problems with AC therapy is not warfarin its the "system". Patients and AC management is patchy and has a bad history. I have come to learn (because I really had to and because with my background I really can) that its overblown unless the patient can not self manage.
did you listen to that presentation? (I know some browsers have issues) Think critically when examining the stats. Look at his graphs and think beyond the cherry picked 15 years (unless you expect to only live 15 years) and stretch out to 20 or more ... suddenly the reoperation rates make rather significant divergances. For instance
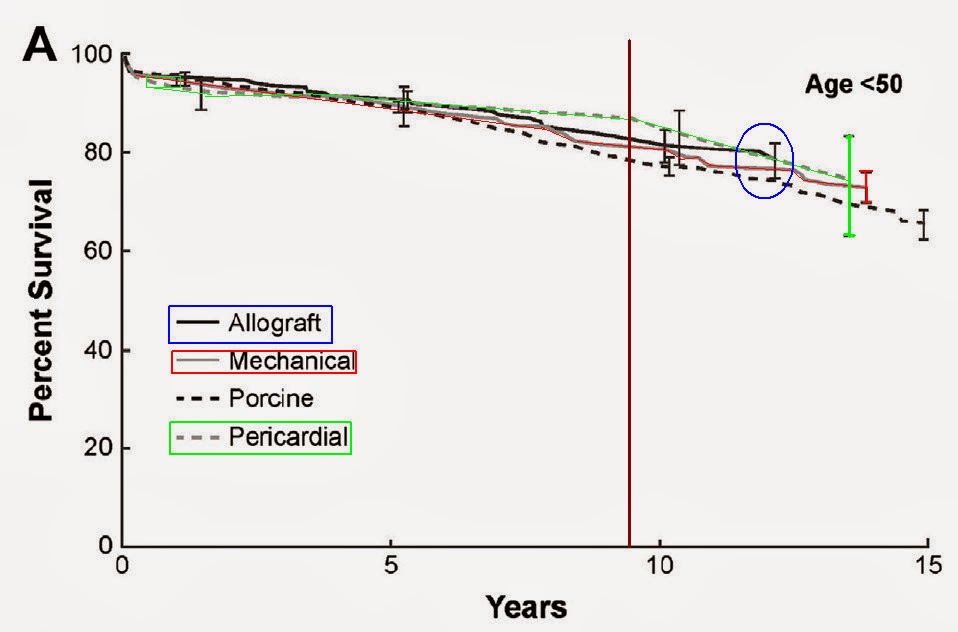
See how they all start together at the beginning of the race but by 15 years all the non-mechanicals are falling by the way. Note also the misleading (which I added emphasis to) statistcial tools to obscure error and undertantity. The Green line (Pericardial tissue prosthetic) has a massive variation in outcome at about 13 years while the mechanical has a much smaller statistical variation in outcomes. Meaning its line is a more reliable indicator and the other lines have much greater variations in outcome.
well that's good in some ways. It to me signals that you are beginning to give up pre-research bias and are now at the point of evaluating evidence based on intellect.
Bottom line
Take the pressure off yourself, relax. Any of the orthodox valve choices are good choices and you will recover and be able to regain life (unlike having no surgery).
Have a think about the points I raised and if you ever feel like chatting PM me and I'm happy to hook up by phone / skype.
Best Wishes
jumpy;n857972 said:The only option that I can see that mimics the hemodynamics of the native valve unfortunately is the Ross.
actually, I agree with your premise - "unfortunately" ... The thing is that too will be a compromise as the tricuspid valve which is removed to replace the aortic valve does not have the same flow characteristics as the aorta, so if your hemodynamics is the key criteria (and please , I'd like to know why it is given so many athletes with mechanicals continue to do well in their sports) then it does not fit either.
Also, I'd be curious to know what you mean by hemodynamics, are you talking about opening / closing perssures, turbulence, closing velocity / opening velocity jets or are you just simply wanting it to carry as much blood?
What data do you have on the various valves and what do you see are the hemodynamic limitations of a modern bileaflet mechanical?
My own gut is telling me to avoid blood thinners but I'm certainly not thinking this over any one issue.
I can understand that, when I had my third valve put in I'd had a sense of dread about blood thinners instilled into me from surgeons in the preceding 20 years (NB from after my homograft). However when the third valve op surfaced suddenly that was brushed aside and "you'll need a mechanical" was all that was really left on the table logically.
I found this worrying, and have come to understand that the key problems with AC therapy is not warfarin its the "system". Patients and AC management is patchy and has a bad history. I have come to learn (because I really had to and because with my background I really can) that its overblown unless the patient can not self manage.
The long term mortality rates are similar for Ross, mechanical and tissue. The re-operation rates that I can see are about 15% for the Ross and 9% for mechanical at 15 years. A broad statistical advantage to be sure but certainly nowhere in the region of tissue which would be closer to 50/50 at 15 years.
did you listen to that presentation? (I know some browsers have issues) Think critically when examining the stats. Look at his graphs and think beyond the cherry picked 15 years (unless you expect to only live 15 years) and stretch out to 20 or more ... suddenly the reoperation rates make rather significant divergances. For instance
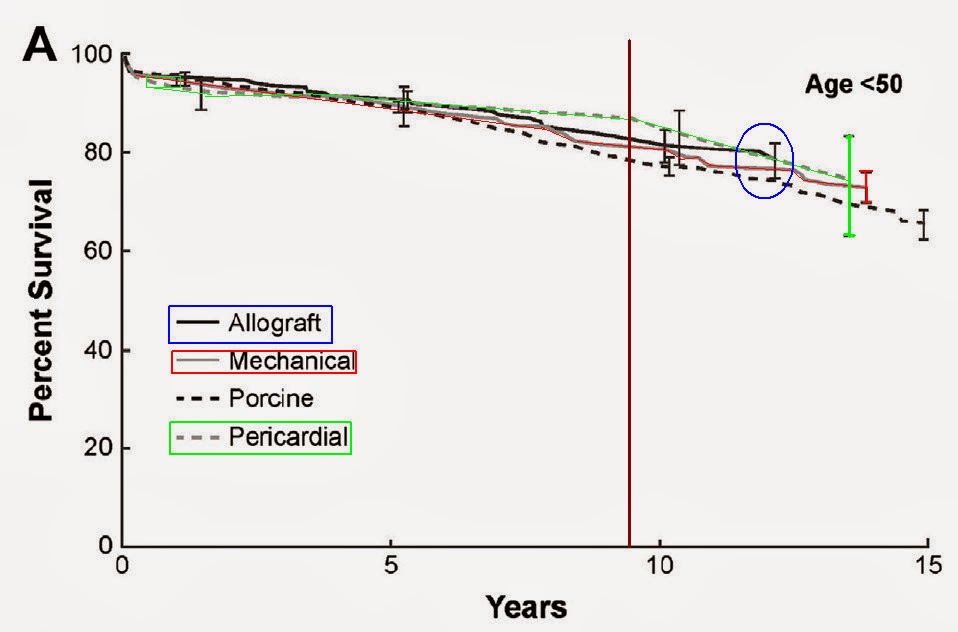
See how they all start together at the beginning of the race but by 15 years all the non-mechanicals are falling by the way. Note also the misleading (which I added emphasis to) statistcial tools to obscure error and undertantity. The Green line (Pericardial tissue prosthetic) has a massive variation in outcome at about 13 years while the mechanical has a much smaller statistical variation in outcomes. Meaning its line is a more reliable indicator and the other lines have much greater variations in outcome.
I meet with the surgeon in a couple of weeks so I want to go in without any decision made but I hope that my questions, his experience/history and my own gut feeling will help me to decide. At this point I feel further from deciding than ever….
well that's good in some ways. It to me signals that you are beginning to give up pre-research bias and are now at the point of evaluating evidence based on intellect.
Bottom line
Take the pressure off yourself, relax. Any of the orthodox valve choices are good choices and you will recover and be able to regain life (unlike having no surgery).
Have a think about the points I raised and if you ever feel like chatting PM me and I'm happy to hook up by phone / skype.
Best Wishes
Thanks. I did listen to the presentation. They did mention a new anti-coagulant but in 2012 it was rejected for use with mechanical heart valves. Otherwise it was enlightening as far as mortality comparison goes. Feels like I'm hunting Unicorns looking for something that may not exist. Being somewhat asymptomatic I've never had to really manage my BAV so it takes some re-thinking.
As I'm now "grounded" I have too much time on my hands to chase myself in circles researching all my choices.
As I'm now "grounded" I have too much time on my hands to chase myself in circles researching all my choices.
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
I found that I took a few listens over a few times to absorb it all. The points are well made about the degradation of tissue and that its not just "X years duration then switch out" its some years of good, followed by some more years of back to life with a failing valve (you being asymptomatic you may not understand what the impact of that is) then a switch out .
Sadly we all wish for the Grail ... but really the options aren't bad. I believe its as much about managing expectations.
I have spent most of my life with this "condition" and after 3 surgeries (with about 20 years between each of them) I think I understand it differently to most.
Well take the pressure off yourself and examine things at leisure. Changing your mind periodically is a good sign as it shows you are considering another aspect. I don't think anyone could realistically expect one to become informed and make this decision in weeks. So much takes time to grapple with.
I try to be a sounding board, and logical. But to be totally open my personal view is that without mitigating reasons to select against anticoagulation therapy that its the best path. Life is about change and we all naturally resist change. If the aversion to ac therapy is really about resisting a change then you should at least be aware of that.
Also, keep in mind that as time goes by we are also running against a wall with antibiotic effectiveness. Post operative infections may well become harder to treat. So while things like TAVI are possible advances in technology s possible that the surgical future may also be fraught.
Lastly, stop thinking of survival and mortality and look at the entire risk and quality of life spectrum. If one (for instance) took a tissue valve which required a reop in 8 years (perhaps less because of your youth) then you got an MSR infection in your redo surgery which required e permanent removal of your sternum, you would not be dead (and be part of that mortality rate number) but life would require a lot more adaptation than a pill once a day. There is bugger all said about that sort of outcome.
I for instance, remain on antibiotics 3 times daily since after my reop in 2011. I got an infection in that surgery. I may be on antibiotics for life. I was lucky, my infection is responding to antibiotics, some don't.
Best Wishes
jumpy;n857976 said:Thanks. I did listen to the presentation. ...valves. Otherwise it was enlightening as far as mortality comparison goes.
I found that I took a few listens over a few times to absorb it all. The points are well made about the degradation of tissue and that its not just "X years duration then switch out" its some years of good, followed by some more years of back to life with a failing valve (you being asymptomatic you may not understand what the impact of that is) then a switch out .
Feels like I'm hunting Unicorns looking for something that may not exist. Being somewhat asymptomatic I've never had to really manage my BAV so it takes some re-thinking.
Sadly we all wish for the Grail ... but really the options aren't bad. I believe its as much about managing expectations.
I have spent most of my life with this "condition" and after 3 surgeries (with about 20 years between each of them) I think I understand it differently to most.
As I'm now "grounded" I have too much time on my hands to chase myself in circles researching all my choices.
Well take the pressure off yourself and examine things at leisure. Changing your mind periodically is a good sign as it shows you are considering another aspect. I don't think anyone could realistically expect one to become informed and make this decision in weeks. So much takes time to grapple with.
I try to be a sounding board, and logical. But to be totally open my personal view is that without mitigating reasons to select against anticoagulation therapy that its the best path. Life is about change and we all naturally resist change. If the aversion to ac therapy is really about resisting a change then you should at least be aware of that.
Also, keep in mind that as time goes by we are also running against a wall with antibiotic effectiveness. Post operative infections may well become harder to treat. So while things like TAVI are possible advances in technology s possible that the surgical future may also be fraught.
Lastly, stop thinking of survival and mortality and look at the entire risk and quality of life spectrum. If one (for instance) took a tissue valve which required a reop in 8 years (perhaps less because of your youth) then you got an MSR infection in your redo surgery which required e permanent removal of your sternum, you would not be dead (and be part of that mortality rate number) but life would require a lot more adaptation than a pill once a day. There is bugger all said about that sort of outcome.
I for instance, remain on antibiotics 3 times daily since after my reop in 2011. I got an infection in that surgery. I may be on antibiotics for life. I was lucky, my infection is responding to antibiotics, some don't.
Best Wishes
almost_hectic
Well-known member
One point that's not been made here regarding a mechanical valve... It's cool to be able to tell people you're a cyborg.
Agian
Well-known member
Hectic, my mother has a knee replacement, a spinal fusion and a pin in her arm. I call her Robocop.
almost_hectic
Well-known member
Agian;n857987 said:Hectic, my mother has a knee replacement, a spinal fusion and a pin in her arm. I call her Robocop.
Exactly! LOL You'll be even more cyborg than her when your time comes.
The thing I always think is so funny about TAVR speculation is that right now, there is a reason they only do this for patients who can't survive open heart surgery. That's because right now TAVR is more dangerous than having them crack your chest open. Just because something is new doesn't make it better. Hopefully over time they will improve the procedure and the balance will shift, but I wouldn't want to be one of the first to sign up. :Scared:
Agian
Well-known member
dornole;n857999 said:The thing I always think is so funny about TAVR speculation is that right now, there is a reason they only do this for patients who can't survive open heart surgery. That's because right now TAVR is more dangerous than having them crack your chest open. Just because something is new doesn't make it better. Hopefully over time they will improve the procedure and the balance will shift, but I wouldn't want to be one of the first to sign up. :Scared:
The high complication rate maybe because most of the candidates are frail to start off. My cardiologist told me that half of all valve replacements in Germany are done through TAVI.
There are lots of (possible) future developments
1) Alternative anticoagulants
2) Mechanical that doesn't require anticoagulation
3) Evolution of TAVI
4) Someone had mentioned Cormatrix, some time ago
... Hope there's more.
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
half sounded like a high amount, so I thought I'd have a little dig around. I found this:
http://www.dhm.mhn.de/ww/en/pub/dhm/..._valve_imp.htm
which is perhaps where the 50% comes from ... 50% of that clinic which seems to specialise in only that ... as 400 procedures per year can't represent all of Germany
Then I dug out this one:
http://www.ncbi.nlm.nih.gov/pubmed/25256201 Sept 2014
so not young ....
it says:
so not good, but doesn't compare to non TAVI
It sums up with:
So again this hardly represents 50% of procedures done ....
Lastly:
http://www.escardio.org/The-ESC/Pre...-to-determine-which-valve-disease-treatment-T
so with nearly twice the death rate "good results" can only be taken in the context of "they had few options"
Ultimately I have to say that I side wit Dornole, its nowhere near mainstream yet, and the complications and stroke rates are only "favourable" when you consider their frail health and advanced age. I wouldn't be lining up to get one even if I could.
Agian;n858002 said:The high complication rate maybe because most of the candidates are frail to start off. My cardiologist told me that half of all valve replacements in Germany are done through TAVI.
There are lots of (possible) future developments
half sounded like a high amount, so I thought I'd have a little dig around. I found this:
http://www.dhm.mhn.de/ww/en/pub/dhm/..._valve_imp.htm
The German Heart Center Munich (DHM) was founded in 1973 and became the first center specifically dedicated to heart health in
Germany.
...
Since 2007, the Heart Team has performed over 500 transcatheter aortic valve
...
This represents one of the largest cumulative TAVI experiences in the world.
We are projected to perform over 200 such procedures during 2010; meaning that about 50% of all our patients with aortic valve
stenosis are now treated with a transcatheter aortic valve implantation procedure.
which is perhaps where the 50% comes from ... 50% of that clinic which seems to specialise in only that ... as 400 procedures per year can't represent all of Germany
Then I dug out this one:
http://www.ncbi.nlm.nih.gov/pubmed/25256201 Sept 2014
Patients in group 2 (n=178, 12% of the overall study population) were older than in group 1 (mean age 82.6±6.3 years vs. 81.6±6.2 years)
so not young ....
it says:
Post-procedural complications were similar in the two groups with 30-day mortality of 6.2% in group 2 compared with 8.3% in group 1 patients
so not good, but doesn't compare to non TAVI
It sums up with:
These preliminary data in a modest number of patients suggest the feasibility of performing TAVI in appropriately selected patients at hospitals without CS but this requires confirmation in future studies involving a large number of patients.
So again this hardly represents 50% of procedures done ....
Lastly:
http://www.escardio.org/The-ESC/Pre...-to-determine-which-valve-disease-treatment-T
[FONT=segoe_uiregular]The reported in-hospital mortality for elective patients was 2.1% for conventional surgery, 5.1% for the transfemoral TAVI and 7.7% for the transapical approach. These numbers confirm the good results of recent studies[/FONT]
so with nearly twice the death rate "good results" can only be taken in the context of "they had few options"
Ultimately I have to say that I side wit Dornole, its nowhere near mainstream yet, and the complications and stroke rates are only "favourable" when you consider their frail health and advanced age. I wouldn't be lining up to get one even if I could.
I'm not at all surprised to read what you have found about that German hospital Pell. I'm always surprised when people are so positive about TAVI. I've a tissue valve and I don't count on TAVI in the future, even a future 15 years down the line, except for people who are "too frail" to undergo open heart surgery. I say that bcause of my understanding of how TAVR is implanted which means the old stenotic valve is still there, albeit, stuck/squashed behind a stent. I do however believe that open heart surgery techniques and anaesthetics and other meds used during surgery will get better and better with time as they always do. The minimally invasive techniques will mean less bone sawing too, especially if the between the ribs technique becomes more widely practiced.
Lawdog
Active member
Double post, sorry.
As a tissue valver, I could probably "sound-of" like a marketing drone for the valve companies. . . but I won't. I will say that I chose a tissue valve at age 63, knowing full well that at some point in my future I could be facing another surgery. Sure, my surgeon (a world-renowned master of the profession) mentioned that TAVI might be in the future, but neither he nor I count on it for me. I made my choice based upon the facts available to me, and based upon how my surgeon and I interpreted them. There are no "givens" in this -- only probabilities. In my case, at age 63, there is a reasonable probability that my valve could last the rest of my life. If it does, great. If not, I will have to play the cards I am dealt at that time. Between now and then, I can live my life as I have chosen, with no regrets.
Why am I saying all this? Just for that last comment -- ". . . no regrets." I believe one of the earlier posters also said it. Just make the best decision you can, then come on back and live your life. Any of the valve choices are good choices. The only bad choice is the choice to do nothing.
Don't be too hard on yourself. Just do your best, then remember that life awaits your return after surgery. . . and so will we.
Why am I saying all this? Just for that last comment -- ". . . no regrets." I believe one of the earlier posters also said it. Just make the best decision you can, then come on back and live your life. Any of the valve choices are good choices. The only bad choice is the choice to do nothing.
Don't be too hard on yourself. Just do your best, then remember that life awaits your return after surgery. . . and so will we.
almost_hectic
Well-known member
By that regard, the same choice made by someone in their 40's like myself, could have to go through the surgery not only more than once but possibly a third time. No thanks


