It's indeed troubling to try to figure out why ONE PERSON apparently has this issue with blood draws and POC machine differences being so large. With the tens of thousands (probably) of comparisons between meters and lab blood draws, and the millions (by now) of INR tests made with meters, it's surprising that one person can encounter this degree of error. I wonder if Roche would like to get involved in figuring it out.
My thought, when suggesting the Coag-Sense meter, was that unlike the others, this meter actually times the formation of a real clot, rather than some electrochemical phenomenon. My assumption would be that the Coag-Sense would get it right--whatever 'it' is. The fact that the Coag-Sense was relatively close to the CoaguChek XS result seemed to suggest that maybe the lab was doing something wrong.
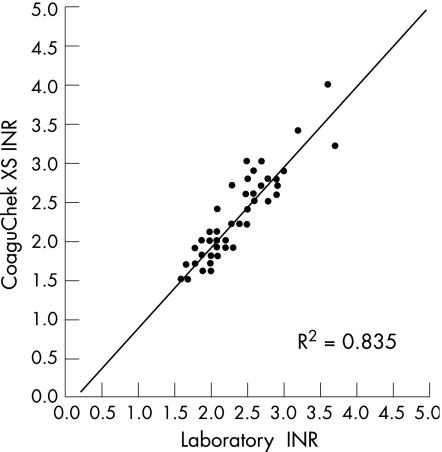
The fact that Linda had blood draws from more than one facility, and there was STILL a fairly large distance between lab and meter is a bit confusing. When testing on my own fingers, I found that the Coag-Sense gave me a value a little BELOW the blood draw, and that the CoaguChek XS (or the XS Plus) gave me a result slightly HIGHER than the lab. In many cases, the lab value was almost an average that of the two meters.
It would be great if this can be figured out and the enigma solved.
For now. because Linda has trouble with vein draws (or, actually, the phlebotomist has trouble finding a good vein), doing a finger stick is much preferred. I'm inclined to suggest (in fact, I AM suggesting) that Linda determines the difference between lab and meter. If the two are consistently different -- either by a specific number regardless of the lab results, or by a percentage above the lab's results -- the meter can still be used for reliable testing. It may be as simple as subtracting the meter's value, or multiplying it by a certain percentage, in order to predict what a blood draw would reveal.
A while ago, there was a formula a formula that could predict a lab's value from an InRatio value was developed. Perhaps a similar algorithm can be developed for Linda, so that she could rely on her meter, with occasional blood draws.
Again, it would be great if the question is solved. in the meantime, if a meter (XS or Coag-Sense) could be shown to be reliably different from the lab value, this may be a good option. (Linda -- you ARE tracking all of this on a spreadsheet, aren't you? Keeping this information handy can be helpful in determining which meter is best, and for demonstrating to your doctors that you're on top of your INR and dosing).
My thought, when suggesting the Coag-Sense meter, was that unlike the others, this meter actually times the formation of a real clot, rather than some electrochemical phenomenon. My assumption would be that the Coag-Sense would get it right--whatever 'it' is. The fact that the Coag-Sense was relatively close to the CoaguChek XS result seemed to suggest that maybe the lab was doing something wrong.
The fact that Linda had blood draws from more than one facility, and there was STILL a fairly large distance between lab and meter is a bit confusing. When testing on my own fingers, I found that the Coag-Sense gave me a value a little BELOW the blood draw, and that the CoaguChek XS (or the XS Plus) gave me a result slightly HIGHER than the lab. In many cases, the lab value was almost an average that of the two meters.
It would be great if this can be figured out and the enigma solved.
For now. because Linda has trouble with vein draws (or, actually, the phlebotomist has trouble finding a good vein), doing a finger stick is much preferred. I'm inclined to suggest (in fact, I AM suggesting) that Linda determines the difference between lab and meter. If the two are consistently different -- either by a specific number regardless of the lab results, or by a percentage above the lab's results -- the meter can still be used for reliable testing. It may be as simple as subtracting the meter's value, or multiplying it by a certain percentage, in order to predict what a blood draw would reveal.
A while ago, there was a formula a formula that could predict a lab's value from an InRatio value was developed. Perhaps a similar algorithm can be developed for Linda, so that she could rely on her meter, with occasional blood draws.
Again, it would be great if the question is solved. in the meantime, if a meter (XS or Coag-Sense) could be shown to be reliably different from the lab value, this may be a good option. (Linda -- you ARE tracking all of this on a spreadsheet, aren't you? Keeping this information handy can be helpful in determining which meter is best, and for demonstrating to your doctors that you're on top of your INR and dosing).