Good day from Kane PA, Its November and no snow yet, Wahoo. I have not been on the forum for a while, but have referred VR.org to several people who have have valves replaced. Things have been going OK, but working with a forester its alot of up and down hills and walking. It seemed to be that it was getting harder, not easier and I would be SOB easier, granted I am older, but the continuous exercise I would think that I should be more able. My GP did a stress test and it showed that I had a blunted heart response and that explained why things are getting more difficult. I made an appointment with my cardiologist, and of coarse he wanted to see this for himself, so we did a stress echo, and my heart actually did pretty good and I went through the entire protocol, but felt malaise for 20 minutes afterwards, which is common for me, I feel crappy after I make a climb up a steep hill, which never happened before. The difference in stress test results, who knows. My cardiologist said my heart didn't respond as he would have expected, my heart is enlarged and he feels that the damage from having regurge for so long before my VR is starting to impact me now as I get older. He didn't really put it in laymans terms what he suspects is going on, but there isn't a whole lot I can do about it. He ordered a Catheterization (which is what this lengthy post is actually about). The hospital in Erie called to confirm my date and told me to stop warfarin 5 days before the cath and no need to bridge. Well this did not sit well with me, I have a big concern with stroking out, 5 days is a long time. Every other surgery I have had, I've always bridged, so I contacted Dr Herrmann, my cardiologist and let his office know what was going on and Hamot saying no need to bridge, just jump off the anti-coag. Well, Dr H ordered me onto Lovenox until the day before, I'd rather have a harder time getting the bleeding stopped, than throw a clot and not know it until something bad happened. Since I walk and climb on a daily basis my heartbeat count is higher that , say an office worker. Ive read where some are getting away from bridging for some minor procedures, my question is what have all of you had for experiences? The members of this forum are the experts as they have lived it so I would appreciate hearing your comments, thoughts/ideas, and experiences. Thank you in advance for your replies, and "Let the Beat Go On"
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Heart Catheterization and stopping anticoagulation for 5 days
- Thread starter westkane
- Start date

Help Support Valve Replacement Forums:
This site may earn a commission from merchant affiliate
links, including eBay, Amazon, and others.
I'd follow Dr. H's advice. 5 days off warfarin without bridging is NOT something I would ever do.....regardless of who thought it might be OK.
W. Carter
Well-known member
I agree with Dick, I would always bridge for at least 5 days before and 5 days after with lovenox shots in the belly. 5 days before stop your warfarin and start lovenox. The morning after the cath start back on warfarin and bridge for at least 5 days. That is how I have done it, your doc may have other idea's.
ALLBETTERNOW!
Well-known member
Recently there was a study out, I can't recall specifics that bridging was not as effective or not bridging was not as risky as they had thought. that being said, I injectected myself as per Drs orde with Lovenox 3 days leading up to checking in for surgery switching off Xarelto
I don't know if there is enough evidence to change the protocol. They are either way out of synch or out in front
I don't know if there is enough evidence to change the protocol. They are either way out of synch or out in front
ALLBETTERNOW!
Well-known member
My schedule was to stop,xarelto 3 days out and then start levenox injection and check in at hospital thereafter they managed me the next day when I had the cath and the following day when I had the surgery. I had a stroke 11 months earlier so was a risk I guess
pellicle
Professional Dingbat, Guru and Merkintologist
ALLBETTERNOW!;n860145 said:My schedule was to stop,xarelto 3 days out and then start levenox injection and check in at hospital thereafter they managed me the next day when I had the cath and the following day when I had the surgery. I had a stroke 11 months earlier so was a risk I guess
When did xarelto gain approval as an anticoagulant for heart valves? The trials were stopped due to deaths IIRC
pellicle
Professional Dingbat, Guru and Merkintologist
Hi and welcome
Firstly if you are going to write so much please use the "enter" key a few times to break it into paragraphs. Its hell trying to read a slab like that.
So you have a mechanical valve (missed it if you mentioned that) and they want to suspend your warfarin for a short time for a procedure?
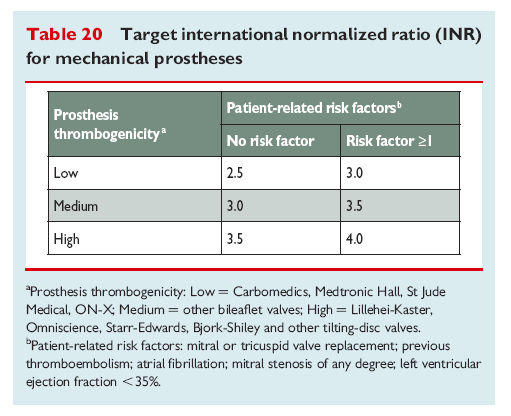
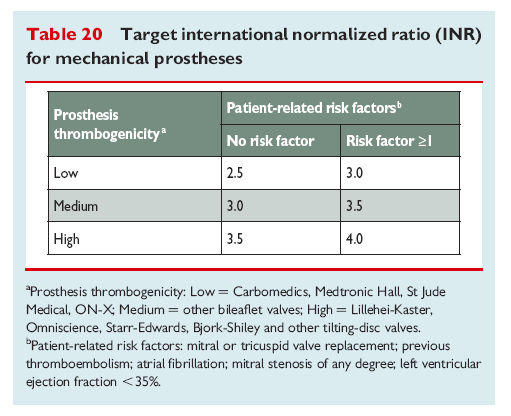
What valve do you have as this alters things. The newer bileaflet valves are apparently less risky to be off for a few days.
See a recent thread here
http://www.valvereplacement.org/foru...518#post858518
(note: perioperative means "around the operation"
Anyway, persoally I have been off warfarin twice since my ATS valve was fitted. Both times for about 3 days, for a surgery. I did not bridge and my surgeon seems to feel that bridging defeats the purpose of going off warfarin.
Best wishes.
westkane;n860138 said:Good day from Kane PA, Its .
...ve read where some are getting away from bridging for some minor procedures, my question is what have all of you had for experiences? The members of this forum are the experts as they have lived it so I would appreciate hearing your comments, thoughts/ideas, and experiences. Thank you in advance for your replies, and "Let the Beat Go On"
Firstly if you are going to write so much please use the "enter" key a few times to break it into paragraphs. Its hell trying to read a slab like that.
So you have a mechanical valve (missed it if you mentioned that) and they want to suspend your warfarin for a short time for a procedure?
What valve do you have as this alters things. The newer bileaflet valves are apparently less risky to be off for a few days.
See a recent thread here
http://www.valvereplacement.org/foru...518#post858518
(note: perioperative means "around the operation"
[FONT=open_sansregular]Do the benefits of anticoagulation outweigh the risks?
The approach to the management of anticoagulation in patients with prosthetic valves undergoing non-cardiac surgery remains controversial. The need for perioperative anticoagulation in patients with mechanical heart valves has been questioned in a recent review. The authors argue that for every 10 000 patients with mechanical heart valves who are given perioperative intravenous heparin, three thromboembolic events are prevented at the cost of 300 major postoperative bleeding episodes.[SUP]3[/SUP] These figures are calculated by assuming an average thromboembolic rate of 8% per year in patients with mechanical heart valves, an anticoagulation-free period of four days and a 3% risk of major postoperative bleeding with intravenous heparin. In light of these calculations, a risk-benefit analysis would preclude the use of full dose anticoagulation during the perioperative period in patients with mechanical valves, except in patients with very recent arterial embolism who have a high risk of recurrence in the absence of anticoagulation. In the absence of recent embolism, the authors recommend, for hospitalised patients, the use of subcutaneous low dose unfractionated or low molecular weight heparin at doses used for prophylaxis against venous thromboembolism, with no prophylaxis for outpatients.[/FONT]
[FONT=open_sansregular]There are limited prospective data to support or contradict these recommendations. The available literature consists mainly of small, non-randomised trials from which no definitive conclusions can be drawn. In one of the few prospective studies, 45 patients with mechanical heart valves underwent non-cardiac surgical procedures.[SUP]4[/SUP] No thromboembolic events were seen in 26 patients with aortic prostheses in whom warfarin was withheld for a total of 6-10 days perioperatively. In 19 patients with mitral prostheses, the warfarin [anticoagulation] effect was reversed with vitamin K on the day of surgery. A heparin infusion was started 12 hours after the operation and warfarin was resumed on the third postoperative day. No thromboembolic events were observed in this group. [/FONT]
[FONT=open_sansregular]Besides being a small non-randomised trial, the other drawback of this study was the lack of long-term follow-up. Valve thrombosis, especially with the tilting-disc (Bjork Shiley) valves, develops slowly and insidiously and may not be evident for 1-2 months. Hence, an uneventful early postoperative period may provide false reassurance that the perioperative anticoagulation has been safe and successful.[/FONT]
[FONT=open_sansregular]A recent review evaluated retrospectively the risk of perioperative bleeding during non-cardiac surgery in 235 patients with mechanical prosthetic heart valves.[/FONT][SUP]5[/SUP][FONT=open_sansregular] A variety of perioperative anticoagulation strategies was used. On multivariate analysis, only a tilting-disc valve in the mitral position and surgery for tumour were found to be predictive factors for a thromboembolic event. Discontinuation of warfarin less than 48 hours before surgery and reinstitution of intravenous heparin within four hours following surgery significantly increased the risk of bleeding. No embolic or haemorrhagic events were detected in 22 patients treated with perioperative low molecular weight heparin.[/FONT]
Anyway, persoally I have been off warfarin twice since my ATS valve was fitted. Both times for about 3 days, for a surgery. I did not bridge and my surgeon seems to feel that bridging defeats the purpose of going off warfarin.
Best wishes.
ALLBETTERNOW!
Well-known member
pellicle;n860146 said:When did xarelto gain approval as an anticoagulant for heart valves? The trials were stopped due to deaths IIRC
Stroke prevention nothing to do with valve as fad as I know
pellicle
Professional Dingbat, Guru and Merkintologist
ALLBETTERNOW!;n860148 said:Stroke prevention nothing to do with valve as fad as I know
you have a tissue valve don't you?
So if I may ask, what is the reason for the stroke prevention, previous history or because of concerns post the aneurysm repair?
(also thank you for quoting me, it gives me a notification and helps me to see amid the forum posts that you replied and that maybe I should follow up)
W. Carter
Well-known member
@ pellicle, I believe if you have a tissue valve and aneurysm vein graft because of the graft material it requires warfarin therapy. I could be wrong. 
They have me as a high risk for clotting because of the vein graft and root surgery. Range 2.5-3.5.
They have me as a high risk for clotting because of the vein graft and root surgery. Range 2.5-3.5.
pellicle
Professional Dingbat, Guru and Merkintologist
InterestingW. Carter;n860178 said:@ pellicle, I believe if you have a tissue valve and aneurysm vein graft because of the graft material it requires warfarin therapy. I could be wrong.
They have me as a high risk for clotting because of the vein graft and root surgery. Range 2.5-3.5.
I have a graft (as well as a mechanical valve) and my surgeon places me as low risk (2.2 ~3)
W. Carter
Well-known member
It could be from the kind of valve I have.pellicle;n860183 said:Interesting
I have a graft (as well as a mechanical valve) and my surgeon places me as low risk (2.2 ~3)
pellicle
Professional Dingbat, Guru and Merkintologist
Your bio suggests a carbomedtric which us a low risk valve. I'm guessing that they are being cautious or you have had some atrial fib . Just based on the valve and the graft you don't seem to qualify for the high risk (which is a good thing)W. Carter;n860199 said:It could be from the kind of valve I have.
ALLBETTERNOW!
Well-known member
pellicle;n860172 said:you have a tissue valve don't you?
So if I may ask, what is the reason for the stroke prevention, previous history or because of concerns post the aneurysm repair?
(also thank you for quoting me, it gives me a notification and helps me to see amid the forum posts that you replied and that maybe I should follow up)
I believe it is due to my prior stroke in Mayn2014. There is actually a healthy debate right now between my cardiologist and surgeon over whether an aspirin is enough or if I should still be on the Xarelto. I don't know anything about Pradaxa but it seems they may have an approved reversal agent pending? I have tolerated the Xarelto well for the last year since the stroke with no know bleeding problems. I was. Allergic to Elliquis when they started me on that right after the stroke. such a fun journey. I also had a maze procedure and don't think I have been in A fib since or for the last year but I have bradycardia and not a racing heart beat A fib, So I never knew I had A fib prior to the stroke or felt it since. I do have a tissue valve and some Dacron in there too.
W. Carter
Well-known member
Thanks that is good to know. My inr will fluctuate from 2.0-4.0. When it is low around 2.0 because I am exercising more than usual I never worry. The cardiology clinic at the V.A. has set me at high risk so I take it with a grain of salt. Although I think they got it from Carbomedics, they are probably just trying to be overly safe. And no I don't have a-fib, never had a stroke, nor have I ever had any clogged arteries, or high cholesterol. Just congenital heart disease (chf), Thanks Mom and Dad!pellicle;n860201 said:Your bio suggests a carbomedtric which us a low risk valve. I'm guessing that they are being cautious or you have had some atrial fib . Just based on the valve and the graft you don't seem to qualify for the high risk (which is a good thing)
Leave it to you to find the good informative stuff on the internet.
Thanks for all the replies, I bridged without a doubt, (sorry for not mentioning I had a St Jude 27AGN put in 2007, which is a butterfly or leaflet design, however my LDH is always in the 550+ range, and my direct billirubin is high, which to me I'm beating the poor RBC's up, St Judes are not supposed to not do that as much as the older versions, however I work with a forester so we make a lot of heartbeats during the day up and down all the hills and valleys compared with say a desk worker.) All the echos, and stress test echos show that the valve is working as it should, no mention of leakage or pannus buildup. Anyway all went relatively well,my legtook about 4 hours to stop bleeding, they put a star closure in. I went to bed but I woke up in the middle of the night with a significant amount of blood everywhere, so here we go again, on my back with pressure for a day, Ive at least stopped bleeding now, but no moving around. I'd rather bleed then have a risk of stroking out. I read the above article about [FONT=open_sansregular]Do the benefits of anticoagulation outweigh the risks? [/FONT]I understand the guts of it, the stats and all, but one bad stroke event may show up in statistics as a very low risk percentage, but that 1% (or whatever % may be), for the person that has the stroke, it is 100% to them. Anyway, thanks to all of you, while I may not visit often ( which is good) you'all are an invaluable source of knowledge, information, and experiences. God Bless to you all and thank again
ALLBETTERNOW!
Well-known member
Best of luck and sorry for your ordealwestkane;n860240 said:Thanks for all the replies, I bridged without a doubt, (sorry for not mentioning I had a St Jude 27AGN put in 2007, which is a butterfly or leaflet design, however my LDH is always in the 550+ range, and my direct billirubin is high, which to me I'm beating the poor RBC's up, St Judes are not supposed to not do that as much as the older versions, however I work with a forester so we make a lot of heartbeats during the day up and down all the hills and valleys compared with say a desk worker.) All the echos, and stress test echos show that the valve is working as it should, no mention of leakage or pannus buildup. Anyway all went relatively well,my legtook about 4 hours to stop bleeding, they put a star closure in. I went to bed but I woke up in the middle of the night with a significant amount of blood everywhere, so here we go again, on my back with pressure for a day, Ive at least stopped bleeding now, but no moving around. I'd rather bleed then have a risk of stroking out. I read the above article about [FONT=open_sansregular]Do the benefits of anticoagulation outweigh the risks? [/FONT]I understand the guts of it, the stats and all, but one bad stroke event may show up in statistics as a very low risk percentage, but that 1% (or whatever % may be), for the person that has the stroke, it is 100% to them. Anyway, thanks to all of you, while I may not visit often ( which is good) you'all are an invaluable source of knowledge, information, and experiences. God Bless to you all and thank again
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
You're welcome
With all that bleeding I would be requesting antibiotic cover ... strongly.
Gail here had a mole removed and the wound weeped for some time. This led to a bacterial colonisation.
I pressed her for her team to implement a VAC bandage (Google that bit of kit) but the insurance was too cheaparse to pay. This is of course not an option for your situation (femural catheter yes?)
If bleeding does not stop very soon I strongly suggest you consider stopping anticoagulant therapy for a short period. Discuss this strategy in earnest with your medical team.
Strike while the iron is hot, do not let it drag out.
Do not underestimate the threat of an infection.
Best wishes.
PS if you are over anxious about stopping AC therapy consider that you miss a dose. That is not uncommon and harmless. Maybe miss two? Ask your team. Dick here missed quite a few with one of the first generation valves, I think that took a week to cause him a problem.
westkane;n860240 said:Thanks for all the replies,
You're welcome
With all that bleeding I would be requesting antibiotic cover ... strongly.
Gail here had a mole removed and the wound weeped for some time. This led to a bacterial colonisation.
I pressed her for her team to implement a VAC bandage (Google that bit of kit) but the insurance was too cheaparse to pay. This is of course not an option for your situation (femural catheter yes?)
If bleeding does not stop very soon I strongly suggest you consider stopping anticoagulant therapy for a short period. Discuss this strategy in earnest with your medical team.
Strike while the iron is hot, do not let it drag out.
Do not underestimate the threat of an infection.
Best wishes.
PS if you are over anxious about stopping AC therapy consider that you miss a dose. That is not uncommon and harmless. Maybe miss two? Ask your team. Dick here missed quite a few with one of the first generation valves, I think that took a week to cause him a problem.
ALLBETTERNOW!
Well-known member
If you are hospitalized or can be watched closely perhaps there is a hedged approach? They can monitor you closely and if you throw a clot they can quickly treat it??? Of course I survived a clot and stroke so I may have a strange view of the risks and potential outcomes
W. Carter
Well-known member
Bridging is a double edged sword. It keeps you from getting clots but it slows healing down alot. Your blood never has a chance to clot long enough to heal fast. I have experienced this first hand after an operation bridging and had doctors tell me it is true. It will heal up, just really slow. Good luck to you.


