I had two thyroid procedures while on warfarin. The first is known as ethanol ablation, which involved a needle draining the thyroid cyst and then another needle inserted to fill the cyst with ethanol, which is then withdrawn after 15 minutes with another needle. My INR range is 2.0 to 3.0 and no holding of warfarin was required, no reduction of INR required and no bridging. My doctor explained that the risk of bleeding was very low with just a needle insertion and no need to hold warfarin. I've had several biopsies done of my thyroid over the years, all before I was on warfarin, and I would estimate that the size of the needles used was similar for the biopsies, compared to the needles used for the ethanol ablation.
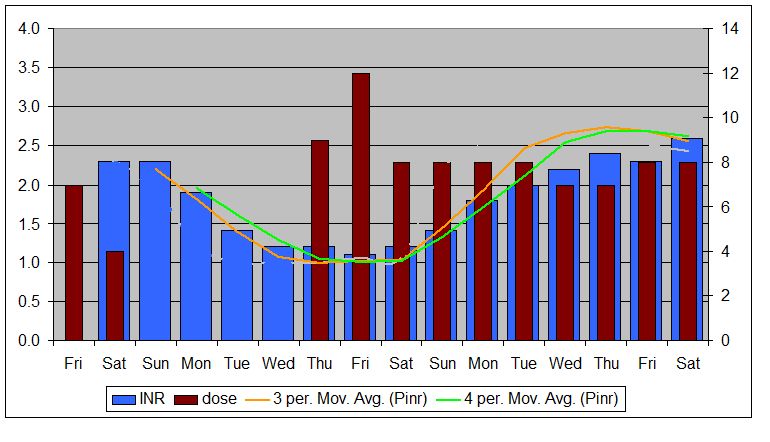
A few months later I had a second thyroid procedure, known as radio frequency ablation. This involved a significantly larger needle, which was used to ablate the remaining thyroid nodule. This was a more involved procedure, with a larger needle, as compared to the biopsies and the ethanol ablation, which had previously been done. Rather than hold my warfarin and bridge, the surgeon had me bring my INR down to below 1.5 before the procedure. As I self test, this was relatively easy to do. I was able to achieve this by reducing my warfarin dosage for a couple of days. Do you self test?
You might want to get another opinion about whether there is a need to hold warfarin and see if they can just reduce your INR, by reducing your dosage. For most procures, especially minor ones like a biopsy, probably getting INR down to 1.5 would be just fine, if lowering is requred at all. For my ethanol procedure, I did make sure that my INR was need the lower end of my range just for good measure.
I would not expect many medical professionals to require bridging for just a biopsy, but they might want to lower your INR a little. Bridging can create some complications and is generally used for more major procedures. I'd be curious as to how long they want you to hold your warfarin. If they want you to hold it for days, I would have a discussion about what the actual INR target is. Some will have a patient hold warfarin for 5 days, to be sure than INR is under 1.5 and then test the morning of the procedure to be sure. For me, personally, knowing how fast my INR drops, this would have been extreme overkill. Ideally, whatever the INR target is for the procedure, you want to spend as little time below that level as possible. This is one very big advantage of self testing, in my view. I was literally able to bring my INR down to 1.4 and just stay at that level for less than 24 hours.