Pellicle,
I have looked at your blog.

followed it from the video you had or one of the other posts. It is indeed pretty detailed and a lot more math than I'm ready for at ANY time! LOL But still very informative. I actually sent it and a few other things I've found on this site regarding home testing to my pharmacist friend, who used to run a AC clinic, and who told me to STAY AWAY from home testing trying to convince him to reexamine his ideas. But that's beside the point to this thread's discussion.

Not sure why the lab tech doing a new finger stick to retest me when initial test came out so high degrades your confidence in him. I think it shows competency because he started over completely just to make sure there were no sampling errors with the first attempt. I don't mean to belabor this point, but it seems to keep being missed.... He is the same one who tested ALL the other patients that day, and ALL their results came out right or as expected. MINE was only one not right. This was checked by the pharmacist AFTER my results were so out of range and so far not in line with the lab results. if he was doing it wrong, the results for EVERYONE would be off, not just mine.
They only made a minor change to my med since my lab INR was a little high of my range, but for most part, have kept things stable. Again, using the lab draw results and not the aberrant POC ones. My concern was with the seeming nonchalance attitude of my cardiologist.
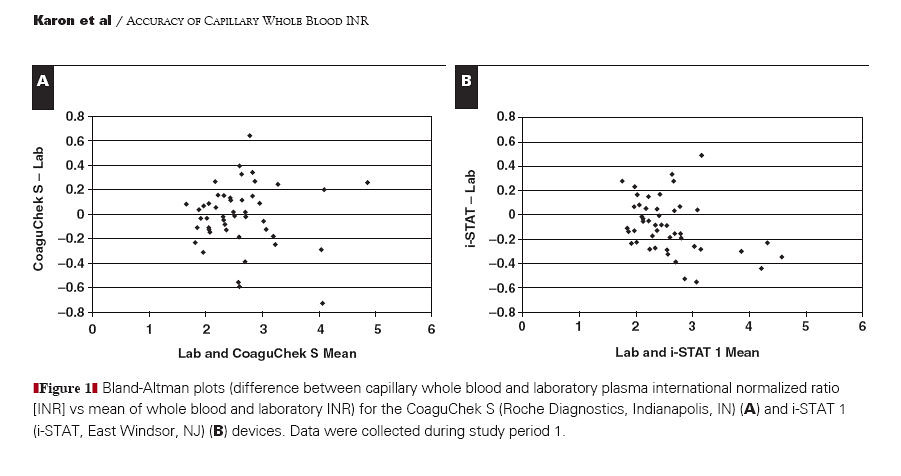
As far as I know, their not using INRatio machines at all. I suspect since this a brand new facility, opened about a year ago, they are using the newer XS machines, assuming I remembered the brand name right. I know it's not INRatio, just not sure if CoaguCheck or CoaguSense. I'll ask again, Wed.
Yes, by lab stick, I mean veinous draw. It almost always takes two or more attempts to draw veinous blood on me, depending on if I get a tech who'll listen to me. Both Antecubital (inside of elbow) areas have scarring from multiple cut downs for Caths that were done on me as a child, so they can't draw from their usual place. This often throws the phlebotomists off right from the start. Then I have small, rolling, tough to enter veins, that collapse as soon as they put the vacu tubes on. They check me on both sides because I'm so hard to even FIND veins on. They do seem to rarely find any on the left, but they always check. Now on top of it all, I'm on Lasix so can't really try to get super hydrated to pump my veins up.... I just pee and pee and pee it out. LOL That's why I really would like to figure out this POC machine issue. I've talked to the head of the lab dept. though, and have a list of their most experienced phlebotomists. So hopefully that will help. I think I'll be off the Lasix soon too, and that will help as well.
To address a couple of your other points:
1. Different branches of the military using different things for same job is VERY common. It boils down to each branch has its own budgets and own acquisition processes, so get different things. Just sticking with the medical side of things, even when the two major military hospitals in just this region supposedly work together, they use different machines or procedures. My Cardiologist sees patients at both facilities (one army, one Navy --- actually joint but let's not confuse things further) but has me redo the Echo at Bethesda (his main office--the Navy one) before my appointments because he knows their machine and their techs better, even if I had JUST had an echo done at the Army hospital on my side of the city and I bring a CD of the actual echo.
Consistency of clinicians is always an issue. Our primary care physicians are in teams of 4 (mix of Drs, PAs, and NPs), so when you call for an appointment, it's just who's available. At least now, I'm complicated enough, that I have my main PMCs actual number and email and can contact her personally if I really need to. Also, reason I'm VERY glad I'm in the AC clinic. They only have two pharmacists (there's another term for them because they're more trained than average pharmacist and can write prescriptions, I just can remember the term); who follow the patients together so there IS consistency of care. They told me on my orientation, to contact them first about any medical issues (colds, procedures, Ect...) and then they will coordinate directly with my Dr. to make sure Warfarin issue is taken into account with any meds prescribed. Nice thing about timing also, is that my Hubby retired last year before all this heart issues happened; so we won't be moving every two years anymore and I won't have to keep re-setting up Drs.
2. I keep a record going on my Ipad with ALL INR results, doses, changes, etc. I've noted each week which number machine was used when I found out there were different machines. Luckily, it'd only been two so was easy to start keeping track from beginning.
3. This brings up a point I figured I'd come across when actually doing home INRs but is sort of salient now. I've seen there are APPS for keeping track of INRs. (Some free, some for small fee)
Some are put out by the various companies and I assume go along with their programs. But others are independent. Do you (and Protimenow) just do your own spreadsheet type records or do you recommend any of the particular tracking options offered commercially?
Well, let's wait and see what happens Wed. I'll come back then with an update.
Linda