This subject has been addressed on other threads, and at other times, but I think it's good to bring it here, where the actual issue can be discussed.
I have St. Jude valve.
I have an InRatio (and a ProTime) INR test machine. I test weekly, unless my INR is out of range (which occasionally happens). If I'm out of range, I make my adjustments and check more often than weekly.
At times, I take a 'weekly' dose that requires a larger dose on some days than on others. I've found that my INR differs, depending on the day I take my INR, based on the dosage I took a few days earlier. On these occasions, although I may be 'in range', my INR is NOT stable. (And, yes, it can vary at different times of the day, and can't be expected to be the same ALL the time).
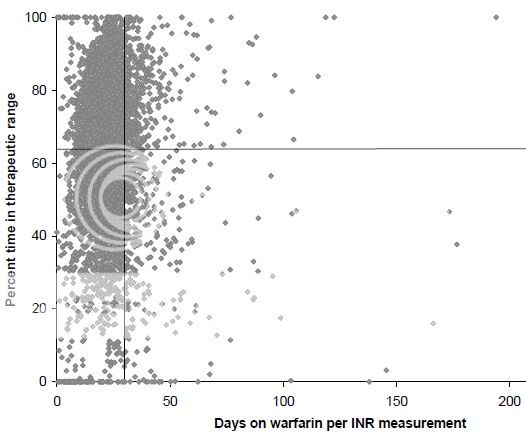
I know that some doctors are satisfied with testing every two weeks (which only tells how the INR is, based on dosage and other factors a few days earlier, but not what happened during the two week lapse.) Others conclude that, if INRs are within range every two weeks for a few months, it's okay to start testing monthly (which, again, allows for a LOT of time to be out of range without having it detected).
At one time, I agreed with these great learned minds. Once I got my tester, I tested weekly (usually).
At one time, testing involved a blood draw. It was expensive and inconvenient, and these factors made it easier to argue against more frequent testing.
Today, with meters available at relatively low cost, and test strips running between $5 and $10, and many warfarin takers able to do testing at home, I don't see the value of increased risk of stroke or embolism when weighed against the avoided cost of an extra test or two (or three) each month.
So I test weekly. I've suggested that others should do the same -- even if they THINK their INRs are stable, and their diets, activities and dosages don't change enough to take their INRs out of range. Not all have agreed.
I expect to get slammed by some who don't agree.
However, I think it may be good to have a conversation about this, and get some other experiences or histories.
I have St. Jude valve.
I have an InRatio (and a ProTime) INR test machine. I test weekly, unless my INR is out of range (which occasionally happens). If I'm out of range, I make my adjustments and check more often than weekly.
At times, I take a 'weekly' dose that requires a larger dose on some days than on others. I've found that my INR differs, depending on the day I take my INR, based on the dosage I took a few days earlier. On these occasions, although I may be 'in range', my INR is NOT stable. (And, yes, it can vary at different times of the day, and can't be expected to be the same ALL the time).
I know that some doctors are satisfied with testing every two weeks (which only tells how the INR is, based on dosage and other factors a few days earlier, but not what happened during the two week lapse.) Others conclude that, if INRs are within range every two weeks for a few months, it's okay to start testing monthly (which, again, allows for a LOT of time to be out of range without having it detected).
At one time, I agreed with these great learned minds. Once I got my tester, I tested weekly (usually).
At one time, testing involved a blood draw. It was expensive and inconvenient, and these factors made it easier to argue against more frequent testing.
Today, with meters available at relatively low cost, and test strips running between $5 and $10, and many warfarin takers able to do testing at home, I don't see the value of increased risk of stroke or embolism when weighed against the avoided cost of an extra test or two (or three) each month.
So I test weekly. I've suggested that others should do the same -- even if they THINK their INRs are stable, and their diets, activities and dosages don't change enough to take their INRs out of range. Not all have agreed.
I expect to get slammed by some who don't agree.
However, I think it may be good to have a conversation about this, and get some other experiences or histories.