New to this thread as Im only 11days post up. Left hospital 2days ago with an inr of 3.4 which had increased from 2.5 two days before, I took 3mg of warfarin both days. I was told not to take any warfain on the day of discharge and only 1m yesterday. My GP tested my inr today and it was 2.0. She advised me to take 1mg for the next 3 days and then we will test again. She also said that while were trying to stabilize the inr im better to be on the low side than the high, which from reading here isn't right. Tempted to take more than she advises, what do people think?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
GP advice? ?
- Thread starter Patsman07
- Start date

Help Support Valve Replacement Forums:
This site may earn a commission from merchant affiliate
links, including eBay, Amazon, and others.
While you're still recovering from surgery (and healing, of course), I would be slightly MORE concerned about clot formation than it sounds like your GP is. Personally, I don't get particularly concerned about an INR of 3.4.
With a 2.0 today, taking 1 mg for the next three days may push you considerably under 2.0.
With the risk of clotting while your body heals, I personally think that it's probably better to shoot a bit higher than a bit lower.
Why don't you call the SURGEON or the Cardiologist and see what THEY advise. They undoubtedly work with this stuff a lot more than your GP does, and may have better advice than your GP, or I, or others on this forum may offer.
In fact, wouldn't it make sense for your cardiologist to be part of the 90 day or so post-op team?
(If you can, get yourself a meter, I use mine for weekly or bi-weekly testing, and compare it to a monthly blood draw. Having your own meter can help you keep on top of any changes, and give you an idea if/when you need to contact your doctor about a questionable value).
With a 2.0 today, taking 1 mg for the next three days may push you considerably under 2.0.
With the risk of clotting while your body heals, I personally think that it's probably better to shoot a bit higher than a bit lower.
Why don't you call the SURGEON or the Cardiologist and see what THEY advise. They undoubtedly work with this stuff a lot more than your GP does, and may have better advice than your GP, or I, or others on this forum may offer.
In fact, wouldn't it make sense for your cardiologist to be part of the 90 day or so post-op team?
(If you can, get yourself a meter, I use mine for weekly or bi-weekly testing, and compare it to a monthly blood draw. Having your own meter can help you keep on top of any changes, and give you an idea if/when you need to contact your doctor about a questionable value).
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
I agree with protime, if in doubt (and your doubt is reasonable) ask around. Ask either your surgeon or your cardiologist if the surgeon can't answer. I realise its a balancing act but where the tightrope ought to be is the main question.
If you feel inclined to self dose (and at those numbers I would) then let the INR management team know that at the next test. Meaning tell them exactly what you too , and probablmthe directions which you went against and why. If your call was right, don't gloat about it too much as that really shits them off when the patient is right.

I agree with protime, if in doubt (and your doubt is reasonable) ask around. Ask either your surgeon or your cardiologist if the surgeon can't answer. I realise its a balancing act but where the tightrope ought to be is the main question.
If you feel inclined to self dose (and at those numbers I would) then let the INR management team know that at the next test. Meaning tell them exactly what you too , and probablmthe directions which you went against and why. If your call was right, don't gloat about it too much as that really shits them off when the patient is right.
My surgeon's office (mainly the nurse) managed my INR for the first month after surgery, then handed me over to my cardiologists care. My GP wants to take over management, and I am reluctant to switch.
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
Depending on some factors it could work in your favor to switch
If yes to most of those you're home and hosed
Best Wishes
My GP wants to take over management, and I am reluctant to switch.
Depending on some factors it could work in your favor to switch
- are you inclined towards self testing?
- will your GP support that?
- are you inclined to self management?
If yes to most of those you're home and hosed
Best Wishes
Just to update. I stupidly went with my GPs advice on Friday, then rang the hospital ward I was on for advice on Saturday. They told me to take 2mg Saturday and Sunday. Got retested yesterday (monday) and my inr was 1.7, which scared me a bit. GP also berated me for not taking the same dose 3days in a row. Have taken 2mg for the past 3days now so hopefully im back up to asafe range
pellicle
Professional Dingbat, Guru and Merkintologist
Patsman
great news that you're back in safe range, however I'm now very curious about the dose you mentioned in the post. I'll assume that its not a mistype when you wrote 2mg as your daily dose.
I wonder if you've been tested for the CYP2C9 and VKORC1 genetic variants, if so I'm curious to know your results, if not then I suggest getting tested will greatly assist in your dosing in future.
Best Wishes
great news that you're back in safe range, however I'm now very curious about the dose you mentioned in the post. I'll assume that its not a mistype when you wrote 2mg as your daily dose.
I wonder if you've been tested for the CYP2C9 and VKORC1 genetic variants, if so I'm curious to know your results, if not then I suggest getting tested will greatly assist in your dosing in future.
Best Wishes
Lots of good advice here. I don't obsess over my INR and test monthly at the cardiologist. Also I'm comfortable with a reading 2-5. The reason I'm even posting is to reinforce the idea that your GP may not be the best to manage your anticoagulant. I have a TOP notch internist and she wanted to change my dose a mg here and a mg there while I was on antibiotics; drove me nuts. Good luck!
Hi
Depending on some factors it could work in your favor to switch
- are you inclined towards self testing?
- will your GP support that?
- are you inclined to self management?
If yes to most of those you're home and hosed
Best Wishes
I'd love to do home testing!
I'm not sure, I've only met him once. I switched shortly after surgery due to piss-poor office staff.
I think I have a pretty good handle on how it all works with my diet/lifestyle.
I'm still new to all of this, and prefer my cardiac RN to manage. I have not yet had three stable readings in a row. 1.7-2.5-4.3-3.1 I'm all over the place!
I've reached my out-of-pocket limit for the year already, so my clinic visits are no charge to me for the next 5 months.
The clinic is a fingerstick with immediate feedback, and the GP is a blood draw and a 2-day later phone call.
Thanks for your advice!
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
well if I understood right you're not long out of surgery, so irregularity is to be expected.
Having said that those numbers aren't so bad.
If you whack that into excel you'll see that its a mean (average) of 2.9 which is a safe level and while your standard deviation is about 1 its also not bad. I've seen higher variance in long-termers who aren't worried about it at all.
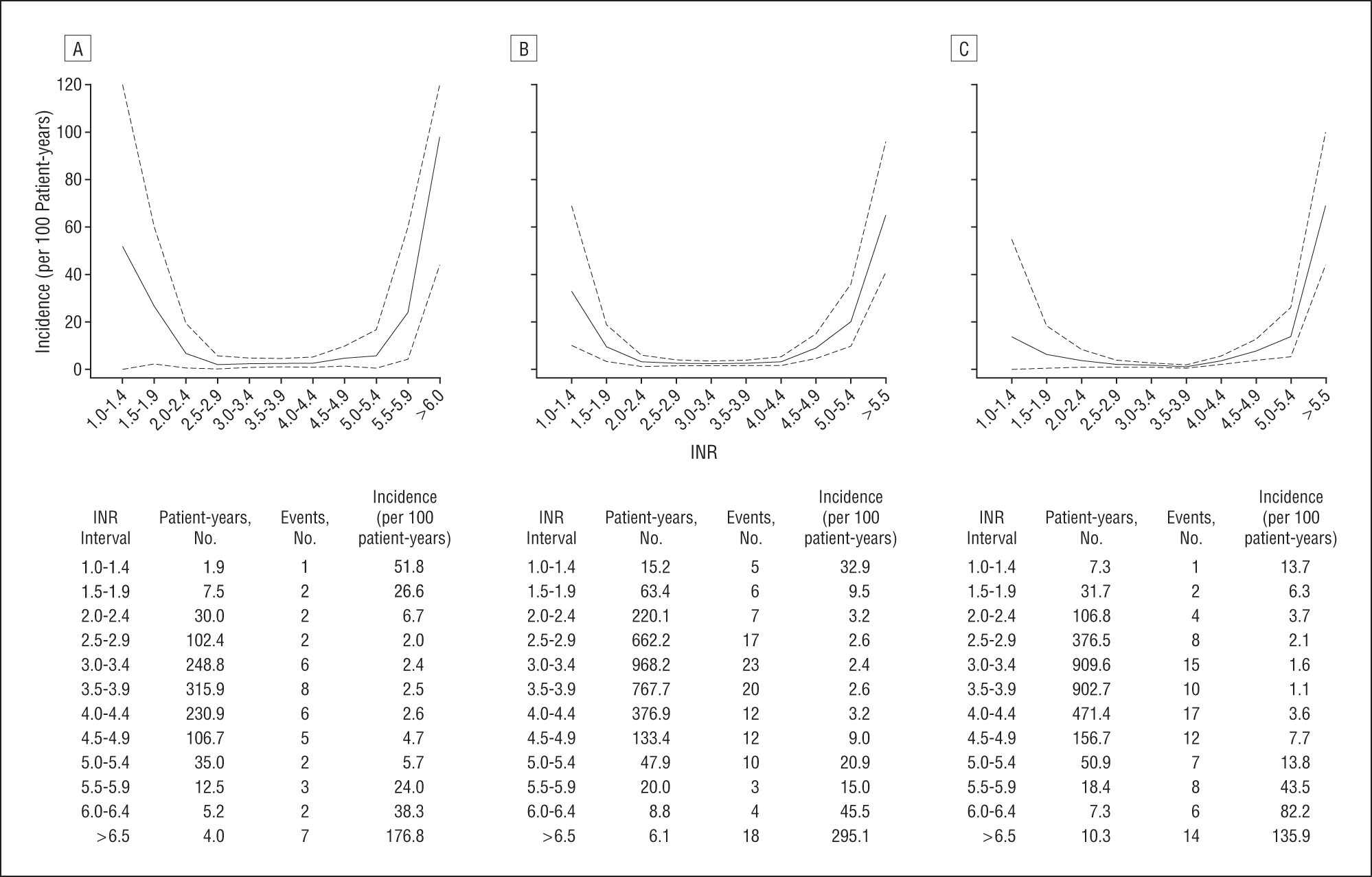
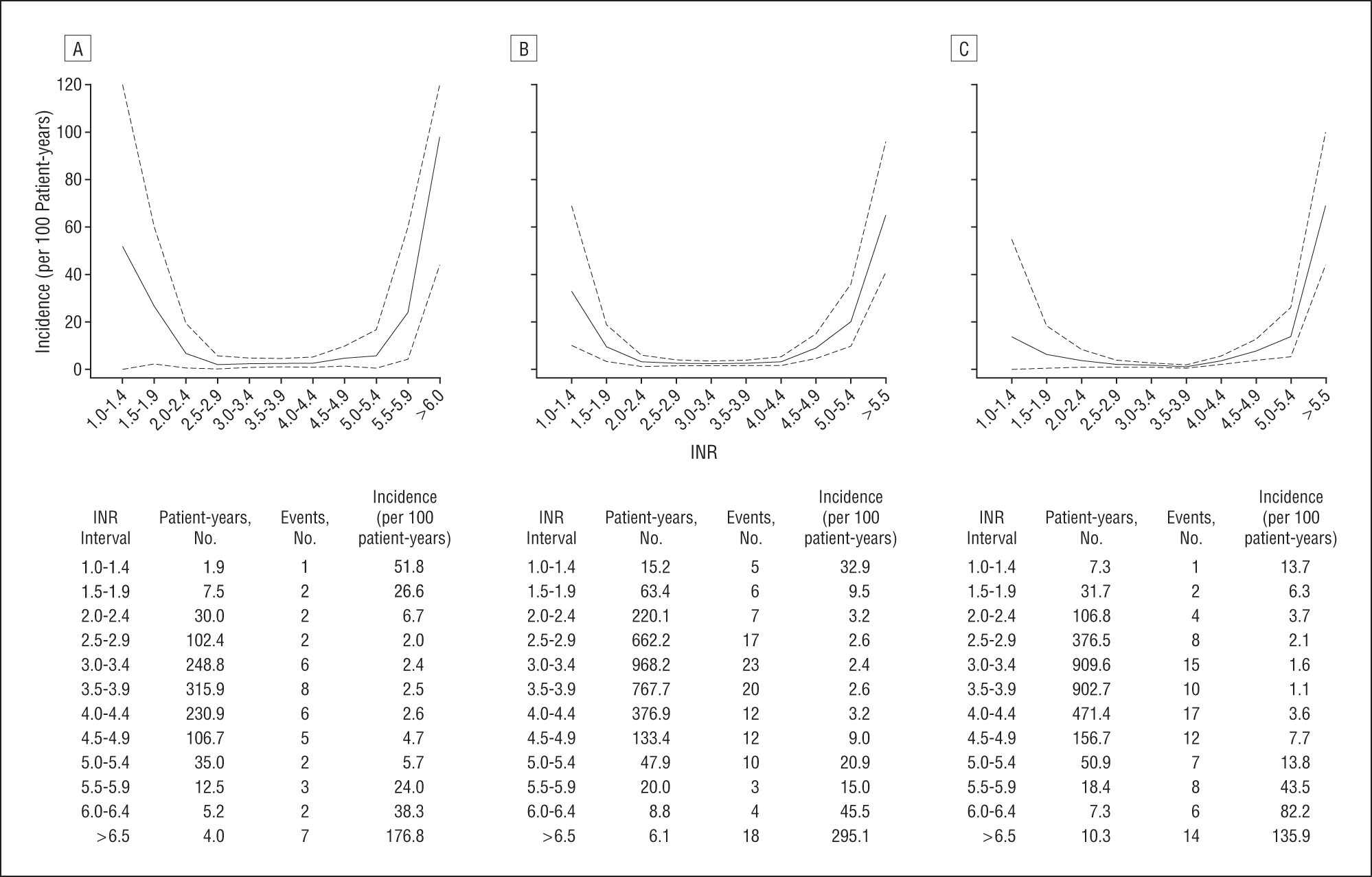
The incidence of issues (such as bleed events) does not really step up till you're over 4.5 For instance, see this graph showing incidence of problems and INR (aortic valve on LHS)
Also, its worth bearing in mind that pretty much no one is flatline "stable" in their INR
I think you're doing fine
I have not yet had three stable readings in a row. 1.7-2.5-4.3-3.1 I'm all over the place!
well if I understood right you're not long out of surgery, so irregularity is to be expected.
Having said that those numbers aren't so bad.
If you whack that into excel you'll see that its a mean (average) of 2.9 which is a safe level and while your standard deviation is about 1 its also not bad. I've seen higher variance in long-termers who aren't worried about it at all.
The incidence of issues (such as bleed events) does not really step up till you're over 4.5 For instance, see this graph showing incidence of problems and INR (aortic valve on LHS)
Also, its worth bearing in mind that pretty much no one is flatline "stable" in their INR
I think you're doing fine
Patsman
great news that you're back in safe range, however I'm now very curious about the dose you mentioned in the post. I'll assume that its not a mistype when you wrote 2mg as your daily dose.
I wonder if you've been tested for the CYP2C9 and VKORC1 genetic variants, if so I'm curious to know your results, if not then I suggest getting tested will greatly assist in your dosing in future.
Best Wishes
I've never had any genetic testing. Would those genes make me more sensitive to warfarin?
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
significantly
http://www.ncbi.nlm.nih.gov/books/NBK84174/
depending on the gene combination 5-7 mg (for what seems to be the highest percentage of the population) to 0.5-2 mg for people with variations of those genes.
Your reported dose was very low (I for instance take 7.5mg per day and I have seen much higher) and so I wondered about this.
Every online dosage calculator (that I have seen) has them and given its so well known I'm rather disappointed (although I will not say surprised) that it is not incorporated into *every* clinics management.
The genes can be determined from the same blood taken to determine INR (if they could be bothered).
Best Wishes
PS:
http://www.warfarindosing.org/Source/Home.aspx
FYI cytochrome P450 is responsible for clearing warfarin from your body and VKORC1 determines how efficient your body is at recycling Vitamin K (which is what warfarin interferes with). Naturally how fast you clear it and how well your body deals with Vitamin K are critical to understanding dosing.
I've never had any genetic testing. Would those genes make me more sensitive to warfarin?
significantly
http://www.ncbi.nlm.nih.gov/books/NBK84174/
depending on the gene combination 5-7 mg (for what seems to be the highest percentage of the population) to 0.5-2 mg for people with variations of those genes.
Your reported dose was very low (I for instance take 7.5mg per day and I have seen much higher) and so I wondered about this.
Every online dosage calculator (that I have seen) has them and given its so well known I'm rather disappointed (although I will not say surprised) that it is not incorporated into *every* clinics management.
The genes can be determined from the same blood taken to determine INR (if they could be bothered).
Best Wishes
PS:
http://www.warfarindosing.org/Source/Home.aspx
his site is supported by the Barnes-Jewish Hospital at Washington University Medical Center, the NIH, and donations. Estimates are based on clinical factors and (when available) genotypes of two genes: cytochrome P450 2C9 (CYP2C9) and vitamin K epoxide reductase (VKORC1).
FYI cytochrome P450 is responsible for clearing warfarin from your body and VKORC1 determines how efficient your body is at recycling Vitamin K (which is what warfarin interferes with). Naturally how fast you clear it and how well your body deals with Vitamin K are critical to understanding dosing.
I used to be comfortable with infrequent testing -- I went for a LONG (stupidly long) time between tests and was lucky not to have had any major events related to this period, but now I get increasingly uncomfortable as my time between tests approaches 10 - 14 days. Weekly testing is a better idea - because a low INR could cause major problems in less than a week. I'd rather catch my INR when it's too low, and correct it with a slightly increased dose than to learn after I've had a stroke that my INR is too low.
(So much for monthly testing).
As far as an internist changing your dose when you are on an antibiotic -- if's not a terrible idea. An antibiotic CAN have an effect on your INR (by killing some of the microbes that have something to do with warfarin absorption, or something), but proactively reacting to the use of an antibiotic is probably not necessary. While on antibiotics, it probably wouldn't hurt to get the INR tested and THEN, if necessary, to make minimal dosing changes. The doctor's advice is not without merit, but probably not necessary for short term antibiotic therapy.
(So much for monthly testing).
As far as an internist changing your dose when you are on an antibiotic -- if's not a terrible idea. An antibiotic CAN have an effect on your INR (by killing some of the microbes that have something to do with warfarin absorption, or something), but proactively reacting to the use of an antibiotic is probably not necessary. While on antibiotics, it probably wouldn't hurt to get the INR tested and THEN, if necessary, to make minimal dosing changes. The doctor's advice is not without merit, but probably not necessary for short term antibiotic therapy.


