Hi
marvsehn;n862060 said:
I am also looking for the right aortic valve. Although I am 64, I am very active. Doing lots of research and have talked with the Docs at Duke Medical and will have a second opinion by Cleveland Clinic. Looks like it is my choice. Either no warfarin and a second procedure 15 years from now or the On-x and warfarin.
something like that ... although pretty much all the pyrolytic carbon bileaflet valves (St Jude, ATS/Medtronics ) have similar profiles. All are good and if a history of performance rather than just "sleek design" is important to you then the StJude has a long history of success behind it.
Every time I think I am close to a decisions more info pops up. the latest is
http://aats.org/valve/presentations/...bio%20AATS.pdf by a Mayo Clinic Dr. This was quite interesting and pointed to use of a mechanical valve for those 50-70. The main point was a longer survival rate after 10-15 years.
indeed ... but I wonder if its because you were thinking tissue prosthesis and the more you learn about mechanical the less problematic they seem? Well a similar report can be found at this URL
http://mayo.img.entriq.net/htm/MayoP...articleID=4071
It opens fine in Firefox but some people have reported problems in Chrome on a tablet (like an iPad).
I've also got a blog post where I outline what I see the major points as being
http://cjeastwd.blogspot.com/2014/01...r-choices.html
Since the On-x valve was approved for lower levels of warfarin (1.5-2.0 INR) in April 2015 I am still looking for info on the ability to manage warfarin in a tighter low range.
Its an intersting point and when first starting out I can see the allure. However my question to you is : does a small drop in range make any difference? I normally manage myself (because I'm that sort of person) and my INR is typically 2.6 My surgeon had suggested to me a range of 2.2 ~ 3 and yet the guidelines are (variously 2~3 or target=2.5
He is of the view that lower INR is correlated to Pannus growth (pretty much the major significant threat to a mechanical valve function). I've not found much research, but surgeons often form opinions on their own experience / conferences and other "unpublished" works. So who knows, maybe 30 years in the field gives them some advantages?
If it is possible then the risk of bleeding should drop!
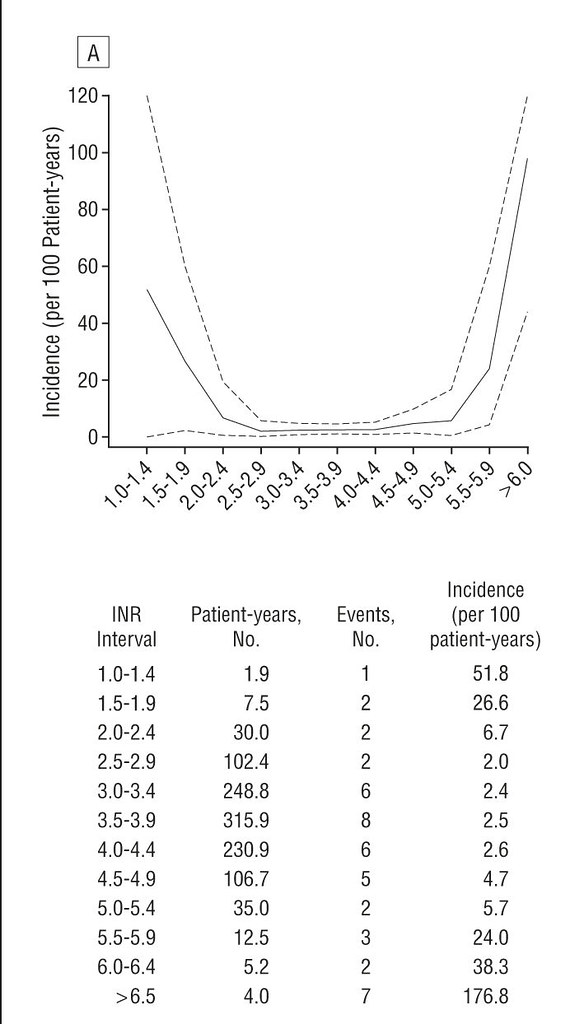
it doesn't quite work like that. The actual risks of bleeding are a function of two things: age and INR. The graph below (from an extensive research paper) shows the reported incidents of problems (clots with INR too low, bleeds too high)
the data shows that you really need to push the threshold of 3 before you see an increase in bleeds
There are other studies (GELIA for instance) showing that all the bileaflet pyrolytic carbon valves are probably conservatively "anti-coagulated" and all (not just On-X) could be safely dropped to a min of 1.7 without problem.
Does this mean a revision of dose? I don't feel that it does. What it means to me is that you can take a consistent dose (which you can determine over time what that is) that sometimes dips you below 2 and sometimes rises you towards 3 without concern to you or your INR manager (and such squiggle in INR is normal).
This also makes life easier for your INR manager (and if you aren't dippy, unreliable, mentally incompetent or senile) then I would argue that that INR manager should be you. Many people (mainly outside of the USA) manage their INR successfully. I'm one who does it not only successfully but does my best to share how and encourage and assist those who do.
I had a dental clean a few weeks back and my dentist always remarks how little I bleed for a fellow on Warfarin. I put this down to effective INR management and that many many many people at clinics have an INR seesaw that they know nothing about (due to poor management).
Some tips on my blog:
http://cjeastwd.blogspot.com.au/2014...ng-my-inr.html
I am also concerned that about 30% of the bio valve people end up on warfarin anyway (for some reason).
well I'm inclined to think that number is a little high, but the causes are varied, with Atrial Fib being one ... other causes are more difficult to "pin down"
So, although I might be leaning to the On-x valve I am still undecided. My surgery date is March 1 so I still have a bit of time.
Good Luck. I will be interested to hear your decision on the valve type and why.
well I didn't "pick" my valve, I got it. My last OHS was my 3rd. I'd had one when I was a kid (to "repair" the valve) another at 28 to put in a homograft, and the last one at 48 to put in a mechanical. I got an ATS and an aortic graft (due to aneurysm). We (surgeon and I) agreed (he told me, I agreed) that a 4th operation would not be at all desirable and that a mechanical gave me the best chance of a long and fruitful life. With a wife and plans for a future I wanted to minimise shocking them and maximise being a good healthy husband for my wife.
Best Wishes