extraordinary
Well-known member
What's your target INR IS IT 2.0 - 3.0 OR IS IT 2.5-3.5 AND why it differs from one person to another ?

What's your target INR IS IT 2.0 - 3.0 OR IS IT 2.5-3.5 AND why it differs from one person to another ?
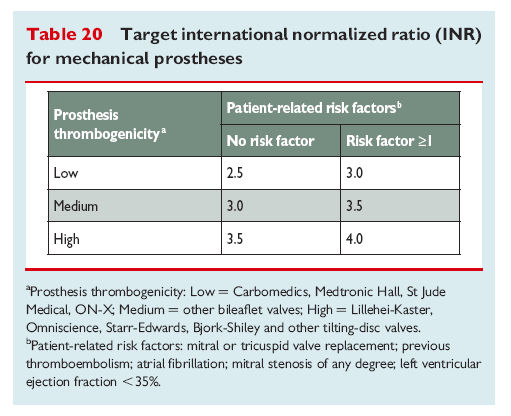
11.2.2.2 Target INR
In choosing an optimum target INR, one should consider patient
risk factors and the thrombogenicity of the prosthesis, as determined
by reported valve thrombosis rates for that prosthesis in relation
to specific INR levels (Table 20).
Currently available randomized trials comparing different INR values cannot be used
to determine target INR in all situations and varied methodologies
make them unsuitable for meta-analysis.
Certain caveats apply in selecting the optimum INR:
† Prostheses cannot be conveniently categorized by basic design
(e.g. bileaflet, tilting disc, etc.) or date of introduction for the
purpose of determining thrombogenicity.
† For many currently available prostheses—particularly newly
introduced designs—there is insufficient data on valve thrombosis
rates at different levels of INR, which would otherwise
allow for categorisation. Until further data become available,
they should be placed in the ‘medium thrombogenicity’
category.
Every doctor I have seen at the hospitals, my GP, etc, all thought the range for a person with a mech AV was 2.5-3.5, and I have had to correct them. I was told by my surgeon that with the On-X aortic valve 2-3 is the target range and that if you had both mitral and AV replaced then its 2.5-3.5.
Had a conversation with the cardiologist's assistant - who didn't even know how to spell On-X and had never heard of it (not very reassuring there again, the folks managing my INR are not even familiar with the mechanical valve that I have or what the recommendations for it are),
Hi
in their defence I would say that its more likely to be surgeons and perhaps cardiologists who know about valve details. The cardiologists assistant is ... well not the cardiologist. To expect them to be as across the business and remain as an assistant would be a bit of a high call.
Also, aside from the marketing calls from On-X I am uncertain that there is any Internationally recognised difference between accepted target INR for bi-leaflet pyrolytic carbon valve. To my knowledge its generally 2.5 target INR.
I can assume that a patient who was given a target of something lower (like 2) and then had a stroke , that said patient may indeed be unhappy and be perhaps inclined to take action against the people involved with managing their INR. So its a case of be cautious. There is very little data supporting anything lower than 2.5 anyway.
Personally I don't see what is to be gained by going "ultra low" in the range other than point scoring value. Can you suggest any benefits to be had by having an INR lower than 2.5 target?
But I digress...this appears to be a learning process for them as well as me.
Since this is the person in the cardiologist's office that is managing patient INRs I would expect that person would be informed (as well as the cardiologist himself) as to what the correct INR ranges should be for the patients/their type of heart valve/etc.
Just the same as I would have wanted the mechanic who worked on my heat pump to know what a TXV valve is (long story).
But that was not the case here, it was just "mechanical valves are 2.5 to 3.5" without knowing/considering anything else like different valves, or different "risk category patients",
And now that they have become familiar with all of that, after consulting with the surgeon and On-x as well, they now feel that my range should be 2 to 3. Being informed is a good thing to help manage patients IMO.
From what I understand, the range is 2.0 to 3.0 in the U.S.
from what I've been reading lately, as approved by some kind of association like the FDA, for the On-X aortic valve, for "low risk" patient factors (sorry but I'm not up on all the details though).
I am not a doctor but as I understand it the benefit is that the lower the effective/safe range for whatever valve it is, the better it is as far as keeping our bodies as close to "normal" as possible,
thus reducing chances of bleeding issues, by not having our clotting times unnecessarily modified to be higher than is necessary, as well as the benefit of reducing other side effects from blood thinners (lower dosages). It's one of the reasons that some people chose biological valves over mechanicals (not having to deal with blood thinners at all).
If a mechanical valve could be invented that required no clotting time modification/no blood thinner med at all wouldn't that be a good thing?
Or if not, then the lower the range the better, because this reduces the chances of clots forming (not having to worry about getting low)?
For example, if a valve is created that studies find cause no clot risk with INR in range of say as low as 1.5, then patients won't have to worry as much about an INR fluctuating down to 1.5 for
PS did I actually manage to figure out how to add a quote!?!?!? Is there an easier way than having to hand delete all the rest of quoted post first? But at least I think I've learned something today.
Yikes! But isn't this SUPPOSED to be the people who are supposed to already know what they're doing?!! Certainly you're not their only patient on AC monitoring!?
My numbers are too low now btw (1.7). Yet he let me go 2 weeks without being tested despite my trying to express that my dosage had previously been upped then dropped, and my numbers were consistently dropping when he took over my "monitoring", and I should be tested more often since I felt I would get too low in 2 weeks. I knew I was going to drop below 2, and keep dropping, and I was right. Sigh.
Well I think that your level of 1.7 is a bit 'dicey' but ultimately it is only you who makes the informed choice on what you feel comfortable with. An old phrase is that its easier to replace blood cells than brain cells (meaning that a small bleed may be less problematic than a small clot and a stroke)
Fatal doesn't bother me in the least, living impaired is quite a serious matter for you and your carers.
Enter your email address to join: