Christ on a bike (No offence by the way I was kicked off an American prayer group loosely disguised as a Heart Forum for such heresy), I do however need to come to a decision I won’t regret.
you just brightened my day right there
Ok ... let me see (probably going to tread on a few toes here, but) here goes:
first lets look at this:
But back to your question I'm 51 so yes Mechanical with the full zipper
please see my response here:
https://www.valvereplacement.org/threads/aortic-valve-choices.887840/page-6#post-907653
of course that wasn't written to you, but I just wanted to clarify that point without typing it again.
very confident with the Edwards Inspiris Resilia Valve
should get you between 10 and 20 years ... ironically the more active you are the less it'll give you. Remeber that just like what you've got now, tissue prosthesis go through a "dying stage" of SVD (see
here for my post and definition)
1. Mini-sternotomy plus Osaki Procedure + Ascending Aorta Replacement may last a long time then TAVI or future variation of.
or may not ... the interesting thing about a mech is that barring another surgical requirement (which would also scuttle the Good Ship Osaki) that choice will last you forever ... and of course the most likely candidate for "redo" with a mechanical is "Aneurysm" which you would appear to be doing now.
2. Ross Procedure with probably median sternotomy, future TVAR or equivalent
sure ... how doses this deal with aneurysm (or have I misunderstood your above point #1?? Why not bugger a perfectly good valve (which may need replacement as Arnie found) to put the wrong valve in the Aortic position? Why would you not go for a cryo preserved homograft of the Aortic valve (and probably get 20 years out of it)??
3. Edwards Resilia plus Ascending Aorta Replacement via Mini-sternotomy. Hope for 15-20 plus years out of the valve
hope ... you sure you can't rejoin that prayer group? And what the heck is it with this mini-sternotomy stuff? Does cutting that bit less bone make so much difference, but
- stopping your heart
- applying you to a machine to ventilate and circulate your blood
- the risks of brain damge (minor that they are) from the above
- the risks of infection (look em up)
all count for nothing? I just don't get this "mini-sternotomy" stuff even figuring in a undergraduate level risk assessment.
then as surgeon stated most if not all valves will be polymer based and replaced via percutaneous methods. Surgeon stated that the Foldax Tria as a TAVR looks promising.
we love trials ... Fusion has looked promising within the next ten years every decade of my life since school (so 1982)
4. Mini-sternotomy proven tech mechanical valve + Ascending Aorta. Replacement in future via less invasive method e.g. right anterior thoracotomy
having already addressed the miniskirt phenomenon and I have no clear idea why you'd need "replacement in future" or why you'd imagine that replacing a mech valve (or any valve) would be "less invasive"
hmm ... ok ... its old, but I'll post it again. Please do watch it carefully and pause or go back 5 sec when you think "wait, what did he say"
pay more strict attention to the stuff on AC Therapy and remember that "home monitoring" (which I do) is even more of a game changer than he anticipated (well, outside the USA mainly, but still).
Then my question to you is "why all the others above 4 ... is it the worry of a pill? Have you searched here on the subject of Anticoagulation?
Here's a blog post which I consider the the prime reference on my blog on the topic
http://cjeastwd.blogspot.com/2014/09/managing-my-inr.html*(edit: corrected the "wrong" link)
you can see that I've had surgeries and procedures on warfarin and when people say "it can be managed" what they mean is (in the main) its trivial.
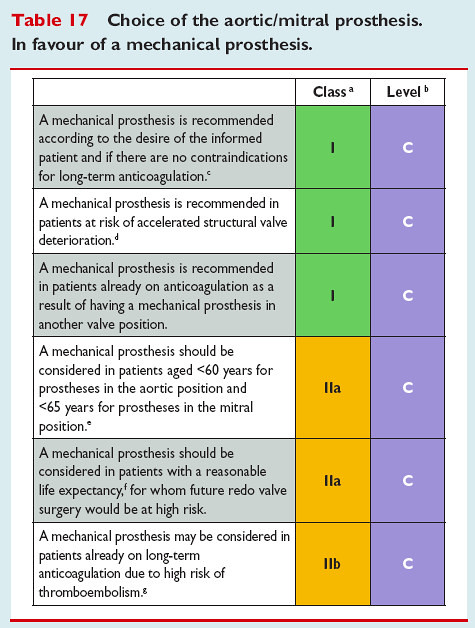
Now, is there some genetic blood disease you haven't mentioned? Because I still feel that nothing has changed since they wrote these guidelines
Bounce back with any "questions" or clarifications.
Best Wishes
PS: just thought ... I know you'll be focused on the now, but for conjectures sake, what do you see yourself doing for the next 20 years (making you 71)? How would you like to be at 70?
I can say after I came home from my second debridement surgery I felt like 5hlt, yet I was only 48. That third surgery was hard, but the infection and its treatments lasted months (Nov through to April) and having only me at home meant when I got back from hospital I was weak and yet had some demanding things to do. It gave me a taste of what it would be like coming home from surgery in my 70's (except that'll be worse). I'll just leave this here to consider
it took a lot of work to get back to XCSkiing again, this is about two years work