Hi
Not cranky, anal I like accuracy. I will take what they give me, but will error on the higher side of the range since the stats show more issues occur with lower INR than higher INR.
noted (although I will remind you that being cranky and moody and slightly illogical (not apparent to you usually at the time) is actually normal)
So let me address a few points
As a background, the calibration of the system (strip is the system, the device is little more than a CD player with the CD being the important part) is done by batch and is what is encoded in that small chip that comes with each batch. The operator is requested to confirm this at the beginning of the test.
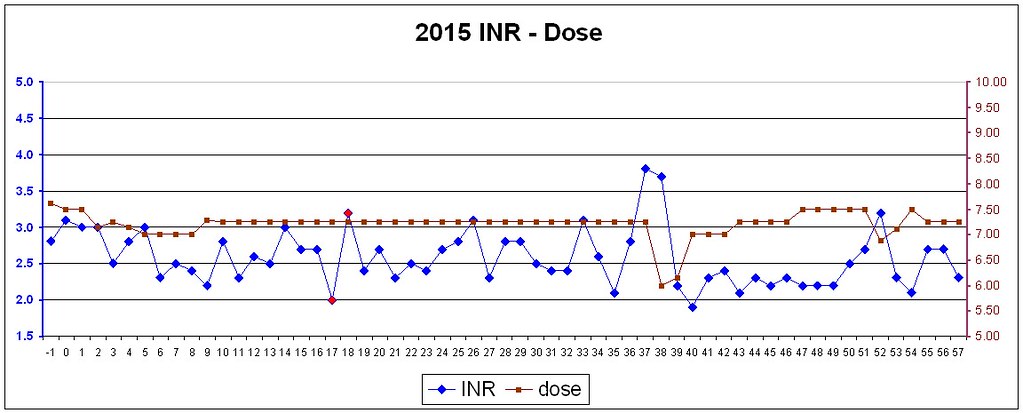
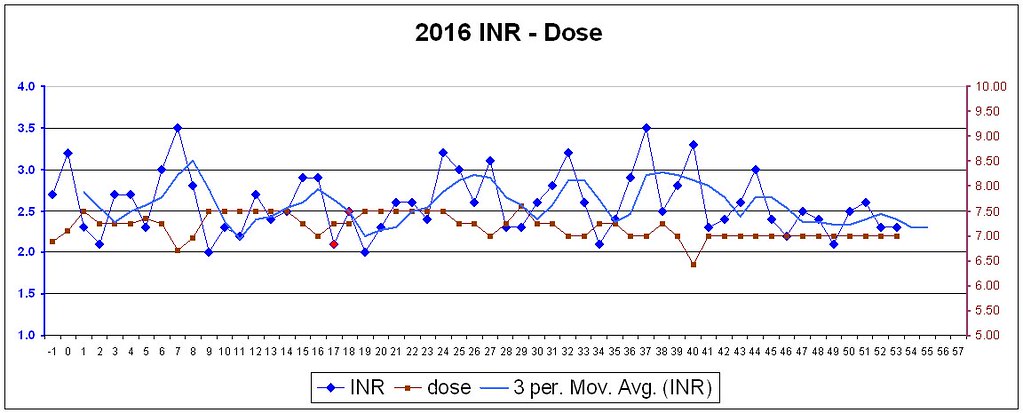
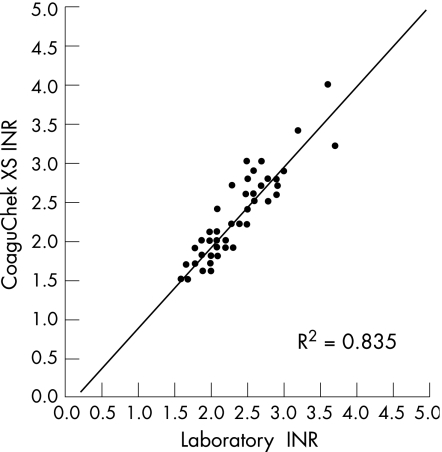
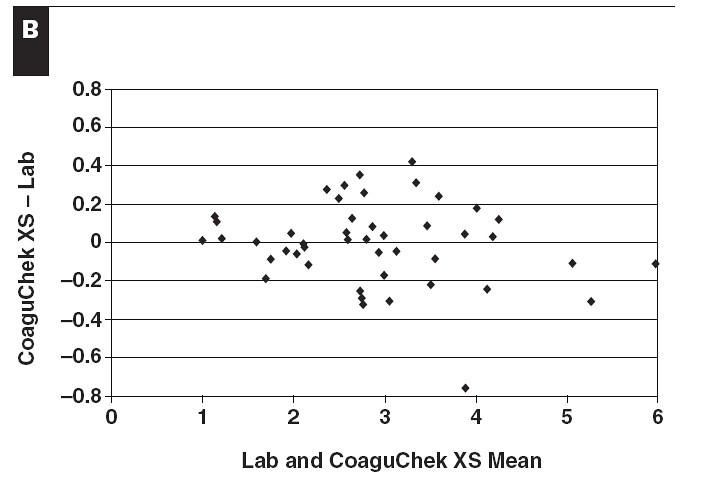
Now, as to accuracy, these graphs are sourced from a study done on the XS system. I would be happy to try to organise getting that study to you if you wish to read it for yourself (if for instance you you may think I'm biased, or you are simply keen to read)
I think they show well that the discrepancy from the agreement from a well calibrated lab result (and be aware that there are many ISI standard reagents that they may wish calibrate against, all of which also have different response curves. So its important to remember you are not dealing with measuring steel with a micrometer here but you are measuring something more nebulous.
With respect to your point about not being cranky and being anal, I'm a software developer of some decades experience. I have worked with major financial institutions developing key (tax) reporting systems and I assure you I know Anal and live it. But your reply seems more like you're cranky to me (of course I don't know you and ASCII tends to mask and distort intention and emotions in the ability of the writer (who may simply be being terse fighting with a phone keyboard) and the reader (who may have phrased the same thing differently).
As I have offered before, if you wish to contact me I'm sure I can provide more support (for at least your informational needs) and assistance in research paths.
Now, as I mentioned before, the introduction of warfarin is a delicate matter with possible (not likely, but hey, neither is surgical infection and I've had that) dire consequences. So they are likely to be taking it prudently.
Your dose is on the high side for introduction to warfarin therapy and so I'm assuming that this has thrown them off their "normal story" and they are unsure how to respond (which btw is simply to keep increasing dose until the "
intention to treat" INR is reached. However they are not specialists they are usually generalists (and there are very few specialists in INR management).
I'm not sure if I've mentioned it before (I recall Warrick saying something and me supporting that, but that may have been someone else) that your INR will not remain stable on that dose (of 7.5) for long and will continue to rise. I think I earlier predicted you will probably settle later on a higher does (so I'll fish out somewhere over 10 right now as a gut feeling).
Warfarin is not like other drugs, it is not dosed by body mass but by your specific P450 response (also influenced by which brand you were started on because different "formula" have different enantiomers of warfarin (see
stereo chemistry and think of your hands) which have different half lives
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1401216/
If I may give a metaphor which is not strictly accurate: Breathing is something we do, but is not something which is "Steady State" depending on what is happening to your metabolism you may breath deeper and faster then other times ... all is designed to keep a very accurate specific level of oxygenation to the blood. Further not all people will respond in the same ways and require different respiration rates to the same "metabolic circumstances"
An introduction to the P450 is possibly well done here:
https://www.ncbi.nlm.nih.gov/books/NBK84174/
If there is laziness in anything its the lack of ever doing these blood tests to understand genotype (which by the way is still being researched in terms of genetic backgrounds of who has them, not their actions) however patient (if one reflects on the other meaning of the word) testing will yeild the best answer anyway, albeit in slightly longer time.
Best Wishes