ElectLive
Well-known member
I'm going to venture a guess that IF I were to conduct a poll, and ask everyone here if they were granted 3 wishes related to the future of heart valves - what they would be, that the final tally might include one or more of the following:
1. Mechanical valve that requires no ACT
2. Tissue valve that lasts forever
3. Catheter (TAVI/TAVR) installed version of either of the above
Well, what if one day, many years from now, you could actually have all three options, but distilled into a single amazing "Valve of the Future"...
My surgeon introduced me to this topic during our first pre-surgery meeting. He had spent 40 minutes or so addressing the nuts and bolts of my case, and had been rattling off inumerable risk/complication rates to the nearest decimal point like only a surgeon can. Then, all of sudden, he threw in a quick little anecdote about what he thought just might change everything for valve patients in the future. He termed it a "hybrid mechanical" valve, inserted by catheter, with a "micro mesh nano technology" of sorts that native tissue would overgrow and engage, including even the leaflets, thus eliminating the need for ACT. Now, I was a little busy at the time planning for my surgery, and quite honestly wasn't on the edge of my seat for a solution 20 - 25 years down the road. So, I never questioned him further about it and just assumed it was likely only in the concept and research stage.
Well, imagine my surprise when I recently read that this mythical valve not only exists firmly in concept, but has also gone through limited animal testing, and is even being mentioned in industry wide (ACC/AHA) literature. In the newly available ACC/AHA "Expert Consensus Document on Transcatheter Aortic Valve Replacement", this formerly nameless (at least to me) "Valve of the Future" is identified and named as a potential next-generation TAVR device by the experts of the profession:
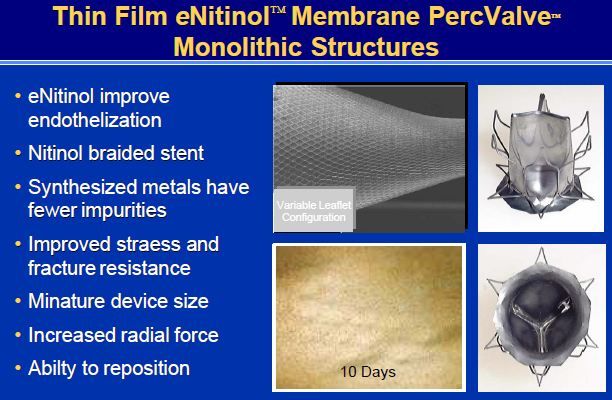
"The PercValve (Advanced Bioprosthetic Surfaces [Palmaz Scientific]) uses nanotechnology in its elastic nitinol frame and leaflets. These leaflets are designed to allow for the growth of endothelial cells, essentially converting it to a tissue valve. Initial animal studies have shown complete endothelialization of the e-nitinol leaflets within 10 days and may eliminate the need for anticoagulation."
Now, if only there were a nano-scientist or nano-engineer with a faulty valve among us who can expand upon this? I certainly am neither, and maybe that's a good thing, because at least that allows me to dream big and think that maybe this is really the idea that will change everything, as my surgeon had said.
Now, assuming it does everything it says it will do, still time for some skepticism. I'm sure there may be reasons why this idea may not translate completely over to the human body. The name behind this PercValve also is not overtly impressive. In other words, if it were the St. Jude PercValve or the Edwards PercValve, it sure would sound a lot more promising and realistic, wouldn't it? Even if were, though, it still obviously would be a long long process (human testing, clinical trials, FDA approval, etc) so a 20 - 25 year estimate (my surgeon's guess) seems pretty fair. Hopefully, though, during that time, the still imperfect world of transcathether valve replacement will also be evolving, and a host of other issues getting worked out (lower profile devices, ability to reposition or retrieve, among others).
Anyway, the world just doesn't change overnight, so all things considered, I still think it's very promising to hear of valve concepts such as this that just might change everything, someday, for valve patients.
1. Mechanical valve that requires no ACT
2. Tissue valve that lasts forever
3. Catheter (TAVI/TAVR) installed version of either of the above
Well, what if one day, many years from now, you could actually have all three options, but distilled into a single amazing "Valve of the Future"...
My surgeon introduced me to this topic during our first pre-surgery meeting. He had spent 40 minutes or so addressing the nuts and bolts of my case, and had been rattling off inumerable risk/complication rates to the nearest decimal point like only a surgeon can. Then, all of sudden, he threw in a quick little anecdote about what he thought just might change everything for valve patients in the future. He termed it a "hybrid mechanical" valve, inserted by catheter, with a "micro mesh nano technology" of sorts that native tissue would overgrow and engage, including even the leaflets, thus eliminating the need for ACT. Now, I was a little busy at the time planning for my surgery, and quite honestly wasn't on the edge of my seat for a solution 20 - 25 years down the road. So, I never questioned him further about it and just assumed it was likely only in the concept and research stage.
Well, imagine my surprise when I recently read that this mythical valve not only exists firmly in concept, but has also gone through limited animal testing, and is even being mentioned in industry wide (ACC/AHA) literature. In the newly available ACC/AHA "Expert Consensus Document on Transcatheter Aortic Valve Replacement", this formerly nameless (at least to me) "Valve of the Future" is identified and named as a potential next-generation TAVR device by the experts of the profession:
"The PercValve (Advanced Bioprosthetic Surfaces [Palmaz Scientific]) uses nanotechnology in its elastic nitinol frame and leaflets. These leaflets are designed to allow for the growth of endothelial cells, essentially converting it to a tissue valve. Initial animal studies have shown complete endothelialization of the e-nitinol leaflets within 10 days and may eliminate the need for anticoagulation."
Now, if only there were a nano-scientist or nano-engineer with a faulty valve among us who can expand upon this? I certainly am neither, and maybe that's a good thing, because at least that allows me to dream big and think that maybe this is really the idea that will change everything, as my surgeon had said.
Now, assuming it does everything it says it will do, still time for some skepticism. I'm sure there may be reasons why this idea may not translate completely over to the human body. The name behind this PercValve also is not overtly impressive. In other words, if it were the St. Jude PercValve or the Edwards PercValve, it sure would sound a lot more promising and realistic, wouldn't it? Even if were, though, it still obviously would be a long long process (human testing, clinical trials, FDA approval, etc) so a 20 - 25 year estimate (my surgeon's guess) seems pretty fair. Hopefully, though, during that time, the still imperfect world of transcathether valve replacement will also be evolving, and a host of other issues getting worked out (lower profile devices, ability to reposition or retrieve, among others).
Anyway, the world just doesn't change overnight, so all things considered, I still think it's very promising to hear of valve concepts such as this that just might change everything, someday, for valve patients.