almost_hectic
Well-known member
No, my cardiologist has upped my range and I now maintain between 2.0 to 2.5Do you continue to be in that same range? Or was that a temporary range?

No, my cardiologist has upped my range and I now maintain between 2.0 to 2.5Do you continue to be in that same range? Or was that a temporary range?
What are the risks. I don’t understand INR . Why would a low INR cause a stroke? I’m trying to learn and really appreciate all of your advice. This is happening so fast and I’m trying to make the right decisions and be as informed as I can be.
Even in Europe, ON-X manufacturer does not indicate as you believe you heard:My cardiologist said in Europe they only take An aspirin a day with an on X valve and are not required to take warfarin. I believe that’s what he said anyway. A lot was said and I’m still sifting through everything in my mind.
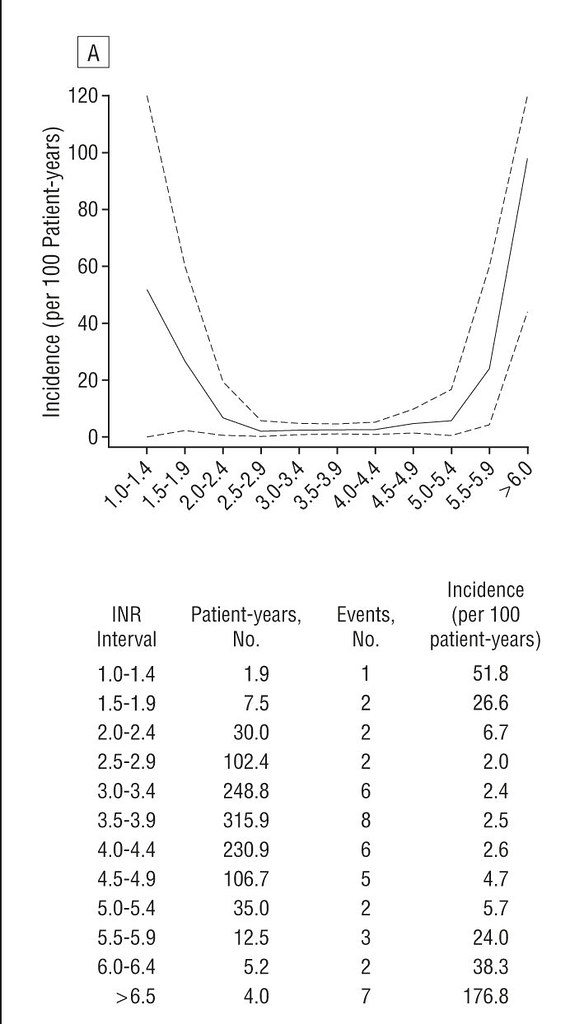
I didn't cite it here because the question was about the On-X and I don't think the On-X is included in that study...@pellicle has the chart supporting 2-4. Don’t know if he posted it in this thread yet, but it’s all over the forum.
it may have been what he said but the reality is (even if he didn't know it) that you MUST take the Aspirin AND take the Warfarin AND keep your INR strictly above the minimum in that range.My cardiologist said in Europe they only take An aspirin a day with an on X valve and are not required to take warfarin. I believe that’s what he said anyway.
nice ... love the wording ... exactly the wording made by Dr Schaff in his presentation ... that its their valve that does this, not the ACT ;-)Even in Europe, ON-X manufacturer does not indicate as you believe you heard:
https://www.onxlti.com/clinical-update-forty-six-recently-approved-europe/
lets not split hairs ... and 2.0 was pretty low too compared to the other ends ;-)Looks like 2.5 - 4.5 is the actual optimal range. My bad.
Well, is a good peace if mind to know that in the event of your INR going below 2 you are safe, mine at the begining went on for 1.5 to 1.9 for weeks, and all went fine. Now after 4 years, i just keep it above 2, so IF it goes down in one of travels to other countries/places, i know for a fact that at 1.6 it works fine, BUT, yes, i do try to keep it at 2.2, and if it goes to 2.5 if fine, and if it goes to 1.6 is fine too, that is how it works " for me", we all have different realms of thoughtThanks everyone for all the great advice. I thought with the on X valve that your INR would be more in 1.5 to 2.0 range. It seems that all of you are more in the 2 to 3 range. Why all the literature and ad campaigns touting a lower INR if nobody is in those ranges??
didn't feel inclined to steer it back up?Well, is a good peace if mind to know that in the event of your INR going below 2 you are safe, mine at the begining went on for 1.5 to 1.9 for weeks,
are you also taking any aspirin?I personally have had around three or four fortunately transient retinal artery occlusions even on Warfarin.
Superman: If your dose alternates between 6 mg one day and 7 mg the next, why don't you just take 6.5? (Yeah - I think I know the answer - it's harder to get a dose of 6.5 than it is to get 6 or 7 - but the answer may be as easy as taking one 4 mg and one 2.5 mg pill per day).
it may have been what he said but the reality is (even if he didn't know it) that you MUST take the Aspirin AND take the Warfarin AND keep your INR strictly above the minimum in that range.
Thanks everyone for all the great advice. I thought with the on X valve that your INR would be more in 1.5 to 2.0 range. It seems that all of you are more in the 2 to 3 range. Why all the literature and ad campaigns touting a lower INR if nobody is in those ranges??
Higher than range or higher than what...don't believe there is any need to keep my INR higher "just in case."
Enter your email address to join: