I'm 8 weeks out from my AVR, (25 mm Edwards Resillia at Cleveland Clinic) aorta graft and CABG x 1. I obsessed over valve choice, and you will too. To simplify, the choice essentially boils down to a biologic that will mimick a realtively healthy native valve (my PCP told me I still have a murmur) that will wear out (10-20 yrs) with a gradual decline in function, no need for a blood thinner (usually), decreased thrombosis risk (when compared to mechanical) vs mechanical that is "one and done" (usually, but not always), lifetime warfarin, audible clicking (some say no big deal, others say an annoyance), increased thrombosis risk compared to the biologic and potential catastrophe in the event of, for example, a serious car accident with open wounds. Rare, yes, but to be considered. I'm 63, so choosing the biologic with a TAVR/TAVI down the road (with luck, 15-20 yrs) was a pretty easy choice. Your "young" age will make the choice more challenging, especially where the trend among surgeons, even at top facilities, is to push biologic, while saying "it's your choice." Best of luck!
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Freshly Hatched and New
- Thread starter Captain Cavemen
- Start date

Help Support Valve Replacement Forums:
This site may earn a commission from merchant affiliate
links, including eBay, Amazon, and others.
- Joined
- Dec 5, 2020
- Messages
- 2,486
I believe the thrombosis risk is equal. In fact, I’m almost certain of this, per the literature. Pellicle will know for certain and will likely have the link to the study regarding this.decreased thrombosis risk (when compared to mechanical) vs mechanical
Hmm... thought that was the reason for the warfarin??
"Thrombotic risk is related to the type of valve, position of the valve and adequacy of anticoagulation," according to Vuyisile T. Nkomo, M.D., M.P.H., director of the Valvular Heart Disease Clinic at Mayo Clinic in Rochester, Minnesota. "Other factors include thrombogenicity of the prosthetic material, shear stress and localized areas of abnormal flow. Therefore, individuals with mechanical valves require lifelong anticoagulation with warfarin along with aspirin, whereas those with tissue valves usually require anticoagulation for only three to six months followed by lifelong aspirin therapy. "
From: Thrombosis of prosthetic heart valves: diagnosis and therapeutic considerations
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1861363/Prosthetic heart valve thrombosis: key points
The latest generation mechanicals, On-X for example, are supposed to present a lower risk, as compared to older generation valves, given the ultra smooth leaflets, which apparently allows for a lower INR. There is also a trial going on assessing whether Eliquis can be used instead of Warfarin, which would siginificant because there is no monitoring, diet restrictions, etc.
"Thrombotic risk is related to the type of valve, position of the valve and adequacy of anticoagulation," according to Vuyisile T. Nkomo, M.D., M.P.H., director of the Valvular Heart Disease Clinic at Mayo Clinic in Rochester, Minnesota. "Other factors include thrombogenicity of the prosthetic material, shear stress and localized areas of abnormal flow. Therefore, individuals with mechanical valves require lifelong anticoagulation with warfarin along with aspirin, whereas those with tissue valves usually require anticoagulation for only three to six months followed by lifelong aspirin therapy. "
From: Thrombosis of prosthetic heart valves: diagnosis and therapeutic considerations
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1861363/Prosthetic heart valve thrombosis: key points
- Prosthetic valve thrombosis (PVT) is a serious complication of valvular replacement associated with significant morbidity and mortality
- The incidence is higher for mechanical than for biological heart valves (right‐sided > left‐sided, mitral > aortic). Non‐obstructive thrombi are more frequently observed than obstructive thrombi
The latest generation mechanicals, On-X for example, are supposed to present a lower risk, as compared to older generation valves, given the ultra smooth leaflets, which apparently allows for a lower INR. There is also a trial going on assessing whether Eliquis can be used instead of Warfarin, which would siginificant because there is no monitoring, diet restrictions, etc.
cldlhd
Well-known member
Obviously I'm not a surgeon but I think it was a great call for them to do your aorta and your root while you were in there. I mean if he thinks it's going to continue to expand then you might as well, I mean who wants another surgery if you can prevent it. It was 6 years ago now but I clearly remember telling my surgeon that I wanted him to do everything that needed to be done or he thought would need to be done while he had the wheels off. I ended up getting the David V , They kept my native BAV and replaced my root ascending aorta and the hemi arch. I've also read a few things that might not apply to your surgery since you had valve replacement but regarding valve repair reshaping and optimizing the valve geometry works better with a root replacement.Great questions.
Prior to surgery, they typically do a CT scan to confirm the aortic diameter of your most recent echo and to measure parts of the aorta that the echo can not accurately measure. This is to determine if you have an aneurysm and will need more than jut a valve replacement. My echo had my aorta at 3.5cm at the root, far below the threshold of needing replacement due to aneurysm. But, when my surgeon opened me up, he looked at my root and determined that the tissue at the 3.5cm point had the appearance that it would continue to enlarge, as happens with a very significant % of bicuspid patients. He is one of the most experienced surgeon's in the country and was going on his experience from completing thousands of similar operations. Even though the textbooks would say that at 3.5cm I did not need my aorta replaced yet, the way I would put it is that this is where the art meets the science. He was using his experience. My wife was in the waiting room and he called her to explain the situation before proceeding- that is a whole other story in itself, but I am already a little long in the tooth, lol.
On my second day in ICU he visited me and fully explained my situation and his decision process in going with the aorta replacement. As I mention above, his experience told him that I was likely to face an increasing diameter of my aorta, by the look of the tissue. He also said that he remembered our lengthy discussions in our two pre-surgery consults and how I changed my mind and wanted to go mechanical because I wanted to be one and done. If I was going tissue, as I would likely be on the operating table again in 10 years he would have left it alone, but since I never wanted another OHS, he decided to replace it now. I told him that he made a world class decision and was so glad that he was my surgeon and that I felt it was 100% the right call.
Per your other questions, yes, when the valve and aorta are both replaced it is called a Bentall procedure. I had a St Jude mechanical valve and he also replaced my aortic root and part of my ascending aorta with a St Jude dacron Hemashield. And, yes, he did it all with a mini-sternotomy, a 3.5cm opening. In my follow up visit with my cardiologist, we both expressed amazement at Dr. Shemin's skill level to be able to do all of that with a mini-sternotomy. The vast majority of surgeon's prefer a full sternotomy and when you talk about surgeon's who are expert enough to complete a Bentall through a mini-sternotomy, you are getting to a very short list- the best of the best. Even if they started with a mini- at that point most would probably shift to a full sternotomy and crack me fully open to give plenty of room to operate. I know that Dr. Shemin is not the only surgeon who can pull this off, as a recent poster recently posted that Dr. Doug Johnson at Cleveland plans to perform his Bentall through a mini-sternotomy. But, he is one of the top surgeons at the #1 clinic in the country. The vast majority of surgeons would not feel comfortable attempting this.
Choosing the right surgeon is very important, and I can't express enough how glad I am that I chose Dr. Shemin. My cardiologist feels that Shemin made the correct call to go with the Bentall. He also said that he believes there might be only about 5 surgeons in the entire US that would have had both the experience to make that judgement call and the boldness to go away from the textbook guidelines at that point.
After my surgery I did some research on the Bentall procedure and was surprised to see that not only are the long term outcomes no worse than those who get just the valve replaced alone, but they are actually better.
I know that you are avoiding reading the published literature at the moment, but if you decide you want to wade back in you should find this study encouraging:
You can skip right to the result if you want the Cliff's Notes version of the study. This is included in the results:
" Long-term survival was 93% after 5 years and 89% after 10 years. Discharged patients enjoyed survival equivalent to a normal age- and sex-matched population and superior to survival reported for a series of patients with aortic valve replacement alone."
I had to read that twice: 5 and 10 year survival for Bentall patients was superior to aorta valve only replacement and the same as the normal population. Remarkable!
https://pubmed.ncbi.nlm.nih.gov/178...al was 93,with aortic valve replacement alone.
P.S. I have no idea how people can go weeks without flossing, I'm not saying I do it perfect floss job every night but I can't stand having food stuck in my teeth....
Last edited:
nobog
Well-known member
The latest generation mechanicals, On-X for example, are supposed to present a lower risk, as compared to older generation valves, given the ultra smooth leaflets, which apparently allows for a lower INR.
Most of the thrombotic "damage" is caused when the mechanical valve is in the closed position due to the high velocity jets. The On-X claims of lower risk are mostly marketing hype.
Most of the thrombotic "damage" is caused when the mechanical valve is in the closed position due to the high velocity jets. The On-X claims of lower risk are mostly marketing hype.
- Joined
- Apr 21, 2021
- Messages
- 13
I can certainly vouch for that. Pellicle has been an enormous help in guiding me towards a stable INR. He has also eased my mind on some of the horror stories that you encounter when you start your warfarin journey. I am very grateful for his time and patience in sharing his knowledge with me.well I can certainly teach you all you need to know to manage INR well if you like my blog is organised by "tags" and this is the full set of tags of INR related articles, should you wish to browse that.
- Joined
- Dec 5, 2020
- Messages
- 2,486
Yes. I should have been more clear. There is no question that without warfarin that mechanical valves are more likely to thrombose. But, since those with a mechanical valve will be on warfarin, the real question is whether a person with a mechanical valve on warfarin is more likely to suffer thrombosis than an individual with a tissue prosthetic, who typically is not on warfarin. I am almost certain that I have seen literature that suggests that an individual with a mechanical valve on warfarin is not at higher thrombosis risk than a tissue valve individual. .Hmm... thought that was the reason for the warfarin??
True. And I believe when properly maintained the risk of thrombosis is no higher for the mechanical valve patient compared to the tissue valve patient. But, don't take my word for it. I will see if I can locate the study when I have some time later today perhaps.Nevertheless, if INR is properly maintained, the risk is very low.
- Joined
- Dec 5, 2020
- Messages
- 2,486
Hmm... thought that was the reason for the warfarin??
I was not able to find the study that I was referring to, comparing mechanical valve thromboembolism vs tissue valve embolism, but I did come across this study which some may find interesting. It studied mechanical valves in the mitral position. During the study there were essentially zero incidence of thromboembolism and bleeding per hundred person years for those in the recommended INR range. Also remarkable is the low number of individuals in range. "INR 2.5–3.4, INR < 2.5, and INR > 3.4 was 41.96, 54.04, and 4%, respectively "
From the study linked below, this graph speaks volumes. From the graph it is clear why they concluded that INR of 2.0 to 3.4 was optimal:

Shown another way:

https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6482495/
Pellicle has posted a study with very similar findings. Staying in INR range = very few events.
And to circle back, the point was made above that a reason to choose tissue prosthetic valve over mechanical is " decreased thrombosis risk (when compared to mechanical) " . As staying in INR range will make thromboembolism events essentially zero, I think that this reason to go tissue should probably not be a deciding factor, unless the individual does not have confidence in their willingness to be consistent in staying in range, which is actually a real consideration. In the above study only about 41% of the participants were in range.
Last edited:
pellicle
Professional Dingbat, Guru and Merkintologist
Indeed, quite similar findings.I was not able to find the study that I was referring to, comparing mechanical valve
..
Pellicle has posted a study with very similar findings. Staying in INR range = very few events.
pellicle
Professional Dingbat, Guru and Merkintologist
Actually here I confess I don't think I've done that one (or did and forgot).Pellicle will know for certain and will likely have the link to the study regarding this.
Let me have a peek
pellicle
Professional Dingbat, Guru and Merkintologist
yes, exactly, however as you note "usually" warfarin is not needed for tissue prosthetic, but because of the "usually" people are blind sided by them throwing clots (and then placed on warfarin), at least with a mechanical we know that's a likelihood and manage around it.Hmm... thought that was the reason for the warfarin??
So to take a step back lets look at this another way. There is no "cure" for valvular heart disease, what we do in surgery is to exchange "valvular heart disease" for "prosthetic valve heart disease". There are two types:
- tissue prosthetic heart valve
- mechanical prosthetic heart valve
- is managed by repeat surgeries, and very occasionally (something in the order of 10%) with ongoing warfarin (for various reasons).
- is managed by warfarin with normally no surgical interventions for the valve itself
The usual decision matrix comes down to the following factors (from the surgical guidelines
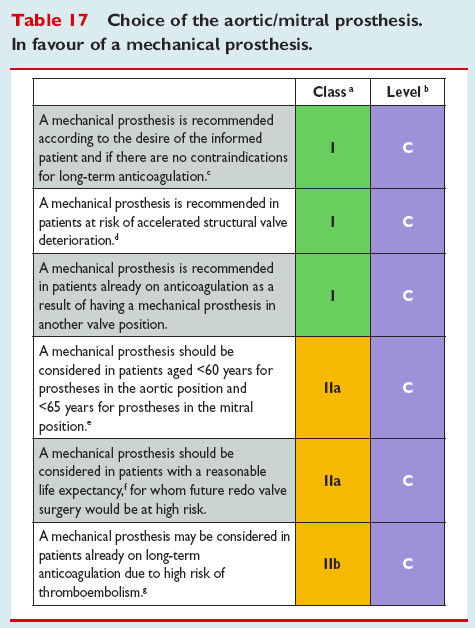
and
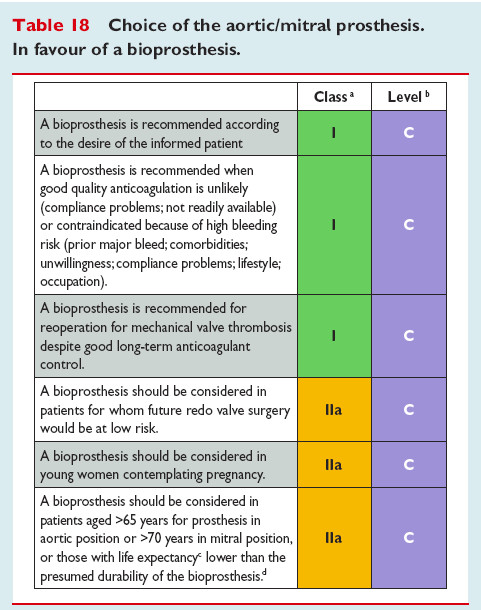
I would read that pair of lists (every word) carefully it is after all not many words.
I note (as did Dr Schaff) that "informed consent" has been placed at #1 position now ... which I think is insane because people are to me becoming insane with the influence of social media and "information" obtained from the internet. (the truth is out there, you just have to know how to sort out the BS)
With respect to warfarin, in the main (unless you are contra-indicated, such as a blood disease, propensity for bleeds ...) I believe its the better option, as one should aim to minimise surgery. Because redo surgery is of increasing complexity and of course risk. Its not just the risk to the heart (such as being on a pacemaker due to nerve damage as nerves often are hidden by scar tissue) but of post surgical infections (just to name one).
Its reasonably well understood that IFF you have a well maintained INR that you are within the usual normal population age related limits of risk for bleeds and thrombosis events (but perhaps protected on long haul flights (if we ever get back to them) form DVT, and maybe clots from the COVID-19 vaccine).
Best Wishes
Last edited:
pellicle
Professional Dingbat, Guru and Merkintologist
an interesting couple of papers
apaper on the topic of bioprosthetic valve thrombosis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306127/
and another on more broad issues (I wonder how many "informed themselves" with this sort of reading, I would hope most)
https://www.ahajournals.org/doi/full/10.1161/circulationaha.108.778886
although I think there are a few editorial issues in that ...
apaper on the topic of bioprosthetic valve thrombosis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306127/
and another on more broad issues (I wonder how many "informed themselves" with this sort of reading, I would hope most)
https://www.ahajournals.org/doi/full/10.1161/circulationaha.108.778886
although I think there are a few editorial issues in that ...
pellicle
Professional Dingbat, Guru and Merkintologist
also, I know its old but:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1767707/
meaning that people with porcine bioprosthetic valves rose over time. I would assume this has to do with Structural Valve Degradation (SVD one shold google that because its not evenly distributed in duration or linear in onset) but its not made clear in that.
So if you picked a tissue valve because you have hang ups about warfarin ... I'm sorry do say that as many as half of you may require it as the tissue valve ages. So if you're hoping to "kick the warfarin can" down the road a bit by having a tissue valve it may be not as much as you're projecting (if you are imagining 20 years and your under 60yo)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1767707/
Exposure to warfarin increased with the passage of time in the porcine group, rising to 33% of AVRs and 57% of MVRs at 15 years postimplant.
meaning that people with porcine bioprosthetic valves rose over time. I would assume this has to do with Structural Valve Degradation (SVD one shold google that because its not evenly distributed in duration or linear in onset) but its not made clear in that.
So if you picked a tissue valve because you have hang ups about warfarin ... I'm sorry do say that as many as half of you may require it as the tissue valve ages. So if you're hoping to "kick the warfarin can" down the road a bit by having a tissue valve it may be not as much as you're projecting (if you are imagining 20 years and your under 60yo)
- Joined
- Dec 5, 2020
- Messages
- 2,486
an interesting couple of papers
apaper on the topic of bioprosthetic valve thrombosis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306127/
and another on more broad issues (I wonder how many "informed themselves" with this sort of reading, I would hope most)
https://www.ahajournals.org/doi/full/10.1161/circulationaha.108.778886
although I think there are a few editorial issues in that ...
Those papers are both excellent resources for anyone in the valve choice process.
An interesting take away comparing the study I linked above and the study you linked regarding bioprosthetic valve thrombosis. BPVT. The mechanical mitral valve study showed thrombosis approaching zero per 100 patient years for those in the recommended INR range. The other study you linked in several other threads had similar findings.
The linked paper regarding BPVT has many referenced studies within it. I'm not going to claim that I read every study linked, but in the ones that I read the rate of thrombosis was not zero- not even close. In the ones which gave the data to approximate incidents per 100 patient years, the rate was actually very high. Certainly high compared to near zero.
This is suggestive that not only would someone with a mechanical valve, with in range INR, be likely not at greater risk than an individual with a bioprosthetic valve, but possibly would be at substantially less risk than said individuals for thrombosis. Of course, the key is "in range INR".
I think this is an important point to make. It was suggested above that a reason to choose tissue valve over mechanical is to have a lower risk of thromboembolism. This is a true statement if the individual is not going to make the very small amount of effort required to stay in INR range. For those who will make that small effort, this should not be a reason to avoid mechanical valves, based on the literature, at least not based on the literature that I have read and that I have seen linked here.
This belief that mechanical valves put a person at higher risk of thromboembolism is widespread. In discussing my valve choice with a physician friend of mine 5 months ago, he asked the question: "Won't you be at higher risk for thromboembolism with a mechanical valve?" It is not his area of specialty- he's an epidemiologist and a lipidologist. But, his question did cause me to look into it at the time and I got back to him that I would not be at greater risk because I would be on warfarin, after reading several papers. This must be why I had that notion in my mind and retracing some of my steps from 5 months ago, I would say that I come to the same conclusion today. But, there are a lot of studies out there and if anyone has a resource that challenges this thinking it would be welcome for them to share the publication. As new data comes in, we should all be open to changing our conclusions.
Last edited:
pellicle
Professional Dingbat, Guru and Merkintologist
agreed and thanks for synthesising the results into a digestible summaryThis is suggestive that not only would someone with a mechanical valve, with in range INR, be likely not at greater risk than an individual with a bioprosthetic valve, but possibly would be at substantially less risk than said individuals for thrombosis. Of course, the key is "in range INR".
cldlhd
Well-known member
I find it hard to believe that in a first-world country people would skip something as important as warfarin when it meant they could have a stroke or die. Don't get me wrong when it comes to other things I can be forgetful or skip them but I can't see how you would with that. The only medications that I'm on is I take an 81 mg aspirin twice a day and I'm on a 40 mg pravastatin. Not sure if I really need that and I'm sure there's 10 different opinions but the cardiologist wants me on it Even though I never had high cholesterol or lipids or triglycerides but two tests back before I knew I had a heart valve issue had me in the high normal range and she believes it should be lower. Point is occasionally I will miss the pravastatin but I don't view that as nearly as important as warfarin is for a mechanical valve. I don't confess to know all of the ins and outs of warfarin, although Pellicle has enlightened me a good bit out here over the years, but I personally can't imagine being relatively young and healthy and choosing a tissue valve knowing I would have to get multiple operations. Maybe if you were a younger woman and wanted to get pregnant I could see it. But as they say it's a personal choice it's just hopefully that choice is made with enough information to make it an educated choice.
- Joined
- Dec 5, 2020
- Messages
- 2,486
I think noncompliance is going to be higher in the third world, for obvious reasons, and will vary country by country, but every study that I have seen has found surprisingly high noncompliance and disappointing numbers for those who have acceptable INR control, regardless of location.I find it hard to believe that in a first-world country people would skip something as important as warfarin when it meant they could have a stroke or die.
This study was done in Saudi Arabia, which has a relatively high per capita income:
Only 46.4% had high adherence to warfarin. This is very low. But, also surprising when they looked at the group that actually complied they found that only 38.2% had acceptable INR control, defined as being in range at least 75% of the time.
" Among the 89 (46.4%) patients who had high adherence, only 34 (38.2%) had an acceptable INR control."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4720013/
Contrast that with Pellicle who diligently self monitors his INR. He tracks his in range statistics and he is in range well over 90% of the time, based on his annual numbers, which he shares with the forum. I self monitor and also am seeing relatively high in range numbers now that things have stabilized for me.
This study tracked Afib patients on warfarin in Northern California receiving care at Kaiser Permanente:
" Within 1 year after warfarin initiation, 26.3% of subjects discontinued therapy "
Like those with mechanical valves, those who discontinue AC therapy with Afib are at risk for thromboembolism:
https://www.ahajournals.org/doi/pdf...tinuation was,range), and patients with lower
So, no doubt the compliance will vary country by country, but even in the first world noncompliance is high and among those who comply, a disappointing number manage to stay in range.
In my view, the take home is when facing the decision as to valve choice, be honest with yourself as to whether you are the type of individual who complies in taking medication and also, by all means, if you choose mechanical, self monitor your INR so that you have better control of staying in range.
I will also add that if you are here on this forum, I would estimate that you are likely more concerned about your health choices and health decisions than the general public and more likely to comply than the average person, but this is just a guess from my observations during my time here.
Last edited:
cldlhd
Well-known member
I agree and I can only speak for me personally But even if I'm not perfect with taking medication at the right time or never missing it I like to think that I have the ability to weigh importance. In other words some medications are more vital to be taken regularly and in compliance than others. Also the stakes are higher with some than others. Also if I thought that doing so would allow me to get a valve choice that, all else being equal, would make it much more likely I could avoid future surgery It's worth the effort. I mean having a second or even a third surgery is rolling the dice a little more often than I would like and also once you get there there's a chance you'll be on warfarin anyway. Don't get me wrong I'm not saying I wish I was on it but basically just saying I think you made the right choice for whatever its worthI think noncompliance is going to be higher in the third world, for obvious reasons, and will vary country by country, but every study that I have seen has found surprisingly high noncompliance and disappointing numbers for those who have acceptable INR control, regardless of location.
This study was done in Saudi Arabia, which has a relatively high per capita income:
Only 46.4% had high adherence to warfarin. This is very low. But, also surprising when they looked at the group that actually complied they found that only 38.2% had acceptable INR control, defined as being in range at least 75% of the time.
" Among the 89 (46.4%) patients who had high adherence, only 34 (38.2%) had an acceptable INR control."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4720013/
Contrast that with Pellicle who diligently self monitors his INR. He tracts in his in range statistics and he is in range well over 90% of the time, based on his annual numbers which he shares with the forum. I self monitor and also am seeing relatively high in range numbers now that things have stabilized for me.
This study tracked Afib patients on warfarin in Northern California receiving care at Kaiser Permanente:
" Within 1 year after warfarin initiation, 26.3% of subjects discontinued therapy "
Like those with mechanical valves, those who discontinue AC therapy with Afib are at risk for thromboembolism:
https://www.ahajournals.org/doi/pdf...tinuation was,range), and patients with lower
So, no doubt the compliance will vary country by country, but even in the first world noncompliance is high and among those who comply, a disappointing number manage to stay in range.
In my view, the take home is when facing the decision as to valve choice, be honest with yourself as to whether you are the type of individual who complies in taking medication and also, by all means, self monitor your INR so that you have better control of staying in range.
I will also add that if you are here on this forum, I would estimate that you are likely more concerned about your health choices and health decisions than the general public and more likely to comply than the average person, but this is just a guess from my observations during my time here.
Last edited:
- Joined
- Dec 5, 2020
- Messages
- 2,486
Agreed. I have taken a few other meds over the years, none of them of vital importance, and I have missed a dose now and then over the years. I've bee on warfarin for almost 12 weeks and never missed a dose- never even taken a dose later than scheduled. That is not to say that I say for certain it won't ever happen over the course of my life, but in that I am very aware of the importance of taking it, I expect I will likely go most years without missing a single dose.some medications are more vital to be taken regularly and in compliance than others. Also the stakes are higher with some than others
But, even with such high stakes, it is remarkable to me the level of nonadherence to warfarin, as shown in the literature, even in developed nations.
I mean having a second or even a third surgery is rolling the dice a little more often than I would like and also once you get there there's a chance you'll be on warfarin anyway.
This is exactly why I chose to go mechanical, after much research and discussion.
pellicle
Professional Dingbat, Guru and Merkintologist
Which makes the greater fitment levels of mechanical valves even more interesting to ponder.I think noncompliance is going to be higher in the third world, for obvious reasons,
I see stupid people everywhere, many don't even know they're stupideven in the first world noncompliance is high and among those who comply, a disappointing number manage to stay in range.

Last edited:


