I make it a personal habit to only assert things which are supportable with robust theory, data or sufficient evidence. I do realise that such is not fashionable
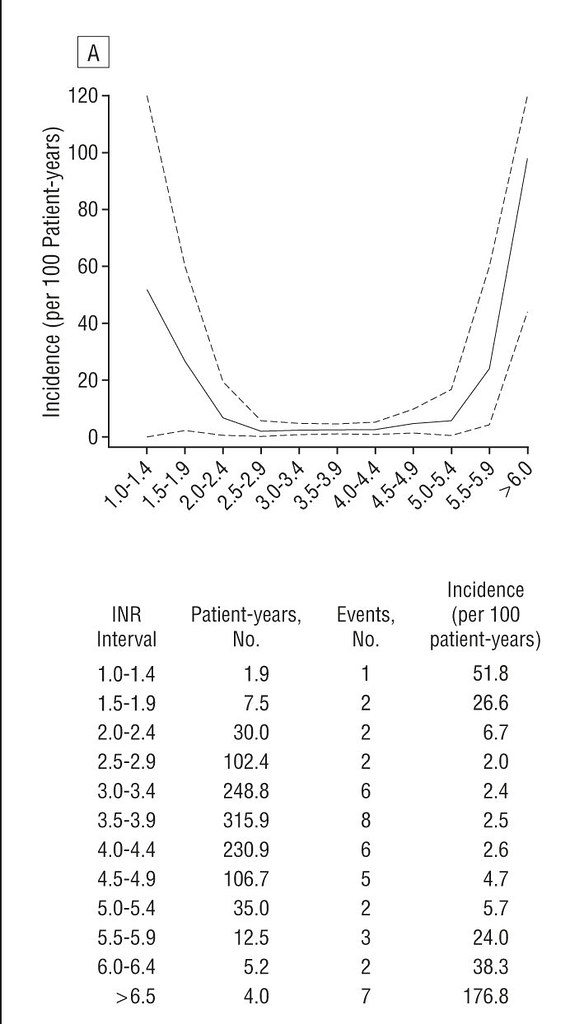
You make it a personal habit to assert that a higher INR is better than a lower one no matter what "Science" in the form of the valve manufacturer and cardiologist say. Your belief in a higher than recommended INR is a personal risk assessment, not based upon empirical data but what "feels good in your gut." I stick to my recommended range of 2-2.5 based upon empirical data and risk assessment done by professional statisticians, cardiologists and medical device engineers.